You searched for:"Carlos Augusto Alencar Júnior"
We found (20) results for your search.Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):53-59
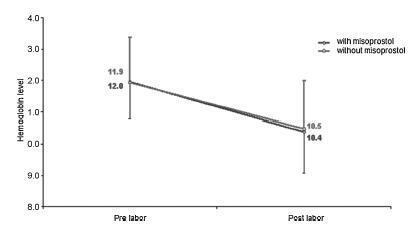
To evaluate blood loss during misoprostol-induced vaginal births and during cesarean sections after attempted misoprostol induction.
We conducted a prospective observational study in 101 pregnant women indicated for labor induction; pre- and postpartum hemoglobin levels were measured to estimate blood loss during delivery. Labor was induced by administering 25 μg vaginal misoprostol every 6 hours (with a maximum of 6 doses). The control group included 30 patients who spontaneously entered labor, and 30 patients who underwent elective cesarean section. Pre- and postpartum hemoglobin levels were evaluated using the analysis of variance for repeated measurements, showing the effects of time (pre- and postpartum) and of the group (with and withoutmisoprostol administration).
Therewere significant differences between pre- and postpartum hemoglobin levels (p < 0.0001) with regard to misoprostol-induced vaginal deliveries (1.6 ± 1.4 mg/dL), non-induced vaginal deliveries (1.4 ± 1.0 mg/dL), cesarean sections after attempted misoprostol induction (1.5 ± 1.0 mg/dL), and elective cesarean deliveries (1.8 ± 1.1 mg/dL). However, the differences were proportional between the groups with and without misoprostol administration, for both cesarean (p = 0.6845) and vaginal deliveries (p = 0.2694).
Labor induction using misoprostol did not affect blood loss during delivery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(1):34-39
DOI 10.1590/S0100-72032012000100007
PURPOSE: To compare the maternal and perinatal outcomes of patients with placenta previa, after the adoption of a prolonged maternal hospital stay, to those of a 1991 series. METHODS: We performed a retrospective study comparing 108 cases of placenta previa hospitalized in the Maternity School Assis Chateaubriand, Universidade Federal do Ceará, during the period from 01/01/2006 to 12/31/2010, with those obtained in 1991, when 101 cases of the pathology were observed at our institution. The following maternal and perinatal data were collected: maternal age, parity, gestational age at delivery, mode of delivery, maternal stay length, Apgar scores at the 1st and 5th minutes, birth weight, adequacy of birth weight, neonatal length stay, maternal and neonatal morbidity and mortality rates (maternal, fetal, neonatal and perinatal). Statistical analysis was performed using the χ² and Fisher's exact tests. The results were considered significant when p<0.05. RESULTS: In 1991, placenta previa was found in 1.13% of cases (101/8900). In the present study, the prevalence was 0.43% (108/24726). No maternal death was observed in either series. Regarding the study of 1991, the current patients were significantly younger, with lower parity, were hospitalized longer, had better Apgar scores at 1st and 5th minutes, and had longer neonatal hospitalization. Also, we identified reduction of fetal, neonatal and perinatal mortality. CONCLUSIONS: Perinatal outcomes in patients with placenta previa were significantly improved between 1991 and the years 2006 and 2010. However, we can not say whether this improvement was due to the prolonged maternal hospital stay.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):361-366
DOI 10.1590/S0100-72032011001100007
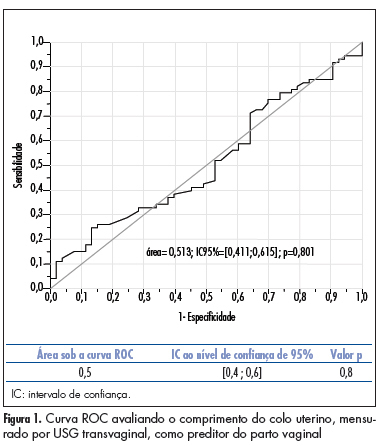
PURPOSE: to compare the accuracy of transvaginal ultrasonographic measurement of the uterine cervix with Bishop’s score for the prediction of vaginal delivery after labor induction, with 25 mcg of misoprostol. METHODS: a prospective study for the validation of a diagnostic test was conducted on 126 pregnant women with indication for labor induction. The patients were evaluated by Bishop’s score and transvaginal ultrasonography for cervical measurement. They also undergone obstetric transabdominal ultrasound to evaluate static and fetal weight, as well as the amniotic fluid index, and basal cardiotocography for the evaluation of fetal vitality. Labor was induced with vaginal and sublingual misoprostol, one of the tablets containing 25 mcg of the drug and the other only placebo. The tablets were administered every six hours, with a maximum number of eight. Frequency tables were obtained, and measures of central tendency and dispersion were calculated. ROC curves were constructed for the evaluation of Bishop’s score and ultrasonographic measurement of the uterine cervix for the prediction of vaginal delivery. RESULTS: the area under the ROC curve was 0.5 (p=0.8) for the ultrasonographic measurement of the uterine cervix, and 0.6 (p=0.02) for Bishop’s score (cut point ³4). Bishop’s score had a sensitivity of 56.2% and specificity of 67.9% for prediction of vaginal delivery, with a positive likelihood ratio of 1.75 and a negative one of 0.65. CONCLUSIONS: ultrasonographic measurement of the uterine cervix was not a good predictor of evolution to vaginal delivery among patients with misoprostol-induced labor. Bishop’s score was a better predictor of vaginal delivery under these circumstances.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(7):352-358
DOI 10.1590/S0100-72032010000700008
PURPOSE: to evaluate the antenatal and postnatal risk factors of neonatal death in pregnancies with absent (DZ) or reverse (DR) end-diastolic flow in the umbilical artery. METHODS: a cross-sectional retrospective study based on data from 48 medical records of singleton pregnancies with DZ or DR, and gestational age of 24 to 34 weeks, at a maternity in the Brazilian Northeast. Mean age was 27.3 (SD: 7.9) years. Twenty (41.7%) patients were primiparas. Hypertensive disorders were found in 44 (91.7%) cases. Thirty-five women (72.9%) had DZ and 13 (27.1%) had DR. Univariate analysis was firstly done (Student's t-test and Fisher's exact test) correlating the parameters with the assessed outcome (neonatal death). Variables that showed significant association were included in the logistic regression model (Wald statistics). The level of significance was set at 5%. RESULTS: The perinatal mortality rate was 64.6% (31/48). There were five stillbirths and 26 neonatal deaths. The mean gestational age at diagnosis was 27.9 (SD: 2.8) weeks. Deliveries before 24 hours after diagnosis occurred in 52.1% of the cases. Cesarean section was performed in 85.4% of the sample. The newborns weighed 975.9 g on average (SD: 457.5). Twenty-four (57.1%) presented Apgar scores below 7 in the first minute and 21.4% in the fifth minute. Gestational age at diagnosis, birth weight and Apgar of the first minute proved to be variables significantly related to neonatal death (p values were: 0.008, 0.004, and 0.020, respectively). The Odds Ratio was 6.6, 25.3 and 13.8 for neonatal death, when the diagnosis was established at the 28th week, weight was <1000 g and first minute Apgar score was <7, respectively. CONCLUSIONS: gestational age at diagnosis, birth weight and Apgar score at the first minute were factors that could predict neonatal death in pregnancies with DV or DR determined by umbilical artery Doppler velocimetry.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(12):639-646
DOI 10.1590/S0100-72032007001200007
PURPOSE: to compare the effectiveness of low doses of vaginal misoprostol (12.5 versus 25 µg) for induction of labor. METHODS: a double-blind, randomized, controlled clinical trial was performed in Santa Casa de Misericórdia de Sobral, from May 2005 to April 2006. Sixty-two term pregnant women, with intact membranes and with indication for labor induction, were included. They randomly received 25 µg (32) or 12.5 µg (30) of vaginal misoprostol each four hours, until the maximum of eight doses. Mode of delivery, time between induction and delivery, perinatal complications, and maternal side effects were studied. The control variables were maternal and gestational ages, parity and Bishop score. The statistical tests used were average calculations, shunting line-standards and Student t-test (numerical continuous variables), chi2 (categorical variables) and Mann-Whitney test (discrete variables). RESULTS: the two groups, 12.5 and 25 µg, did not differ in relation to the interval of time between the induction onset and delivery (1524 versus 1212 min, p=0.333), in the frequency of vaginal delivery (70 versus 71.8%, p=0.720), Apgar scores below seven at the fifth minute (3,3 versus 6,25%, p=0.533) and tachysystole frequency (3.3 versus 9.3%, p=0.533). The average of total dose administered was significantly higher in the 25 µg group (40 versus 61.2 µg, p=0.03). CONCLUSIONS: vaginal misoprostol in the dose of 12.5 µg was efficient, with collateral effects similar, to the 25 µg of vaginal misoprostol, for induction of labor at term.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(8):481-484
DOI 10.1590/S0100-72031998000800009
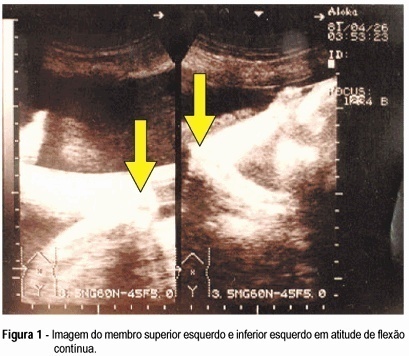
Arthrogryposis multiplex congenita is characterized by multiple joint contractures present at birth. Prenatal diagnosis is difficult. There are few reports in the literature. Fetal akinesia, abnormal limb position, intrauterine growth retardation, and polyhydramnios are the main findings of the ultrasonographic diagnosis. The authors describe a case of arthrogryposis multiplex congenita ultrasonographically diagnosed in the third gestational trimester. The main findings were absence of fetal movements, polyhydramnios, symmetrical and non-symmetrical fetal growth retardation with marked decrease of abdominal and thoracic circumference, low-set ears, micrognathia, continuous flexure contracture of limbs, internal rotation of the femur, and clubfoot on the right.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(7):377-379
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(7):410-415
DOI 10.1590/S0100-72032006000700006
PURPOSE: to verify, through pelvic ultrasound, the existence of changes in the internal genitalia of girls with central precocious puberty, submitted to treatment with gonadotrophin-releasing hormone (GnRH) analogs. METHODS: pelvic ultrasound was performed in 18 girls with idiopathic central precocious puberty, before and after three months of onset of the treatment with GnRH analogs, to investigate the impact of the therapy on the internal genitalia. Ovarian and uterine volumes, uterine longitudinal length, relation between the longitudinal diameter of the uterine corpus and the uterine cervix, the relation between the anterior-posterior diameter of the uterine corpus and the uterine cervix, and endometrial echogenicity were evaluated. Statistical analysis was performed through Shapiro-Willkis's test, to assess data normality. When normality was present, Student's test t was applied. For data without normality, a non-parametric test (the signal test) was used. RESULTS: after therapy, statistically significant decline of the mean uterine volume (from 5.4 cm³ to 3.0 cm³, p<0.001), of the mean ovarian volume (from 2.2 cm³ to 1.1 cm³, p= 0.004), of the mean uterine longitudinal length (from 4.2cm to 3.4 cm, p=0.001), and of the mean endometrial echogenicity (from 1.8 mm to 0.6 mm, p=0.018) occurred. CONCLUSION: In girls with idiopathic central precocious puberty, pelvic ultrasound is a valid method to assess the efficacy of treatment with GnRH analogs. The main parameters of the therapeutic response were the decrease of uterine and ovarian volume, of uterine longitudinal length, and atrophy or absence of endometrial echogenicity.