Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):436-436
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):373-375
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):382-386
DOI 10.1590/S0100-72032005000700003
PURPOSE: to evaluate periodontal conditions and need for treatment supplied by Periodontal Screening and Recording (PSR) in mothers, in order to clarify the relationship between periodontal disease and low birth weight premature newborns. METHODS: PSR was used in a sample of 40 mothers, divided into: test group, consisting of mothers of premature newborns with weight less than 2,500 g (n=20), and the control group, consisting of mothers of term newborns with a weight equal to or over 2,500 g (n=20). The collected data were analyzed by descriptive statistics, and the results of PSR were submitted to statistical analysis in order to verify differences in periodontal condition and need for treatment of the mothers, using the Kolmogorov-Smirnov test, with a significance level of 5%. RESULTS: the presence of periodontal pocket of 3.5 to 5.5 mm was the most common finding among the mothers of newborns with low weight (39.2% of the cases), while the presence of bleeding at probing and absence of a periodontal pocket were the most frequent findings among the mothers of newborns with normal weight (37.5% of the cases). There was a statistically significant difference between periodontal conditions of the mothers of the groups (p=0.0494), but in relation to the need for treatment, there was no significant difference between the studied groups (p>0.05). CONCLUSION: the mothers of preterm newborns with low weight presented worse periodontal conditions, suggesting that periodontal infection may be related to preterm low birth weight newborns.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):387-392
DOI 10.1590/S0100-72032005000700004
PURPOSE: to assess peak systolic velocity (PSV) and the resistance index (RI) in the middle cerebral artery (MCA), suprarenal aorta (SRA) and infrarenal aorta (IRA) of the fetus and in the umbilical artery (UA) between the 22nd and 38th week of gestation. METHODS: a prospective study which evaluated the parameters of 33 normal fetuses in the 22nd, 26th, 30th, and 38th week of gestation. Pregnant women with a singleton fetus with no diseases or complications and who agreed to participate were included in the study. Exclusion criteria were fetal malformations, discontinuation of prenatal care visits and mothers who smoked, used alcohol or illicit drugs. Ultrasound examinations were performed by a single observer. For the acquisition of the Doppler velocimetry tracing in the MCA, SRA, IRA and UA, the sample volume was 1 to 2 mm, placed in the center of the arteries. The insonation angle was 5º to 19º in the MCA, below 45º in the SRA and IRA, and less than 60º in the UA. We used a wall filter of 50-100 Hz. The parameters were calculated automatically with the frozen image, three measurements being made. The final result was obtained by the arithmetic mean of the three values. Data were analyzed by analysis of variance (ANOVA), post hoc Bonferroni test, Pearson's correlation, and regression analysis. The level of significance was set at p<0.05 in all analyses. RESULTS: PSV increased from 26.3 to 57.7 cm/s in the MCA between the 22nd and the 38th week of gestation (p<0.05). In the SRA and in the IRA, PSV increased between the 22nd and 34th week of gestation, from 74.6 and 59.0 cm/s to 106.0 and 86.6 cm/s, respectively (p<0.05). In the UA, PSV increased between the 22nd and the 34th week of gestation, but decreased from 55.5 to 46.2 cm/s between the 34th and the 38th week of gestation. In the MCA, the RI was lower in the 22nd (0.81) and 38th week of gestation (0.75) and higher (0.85) in the 26th week (p<0.05). In the SRA, the RI values were stable in all weeks and in the IRA they were stable in most weeks (p>0.05). In the UA, RI decreased from 0.69 to 0.56 between the 22nd and 38th week of gestation (p<0.05). CONCLUSION: in normal fetuses, in the second half of gestation PSV increased in the MCA, SRA and IRA, decreasing in the UA between the 34th and 38th week of gestation. RI was lower in the 22nd and 38th weeks of gestation in the MCA, decreased between the 22nd and the 38th week in the UA, and was constant in most of the gestational weeks in the SRA and IRA.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):393-400
DOI 10.1590/S0100-72032005000700005
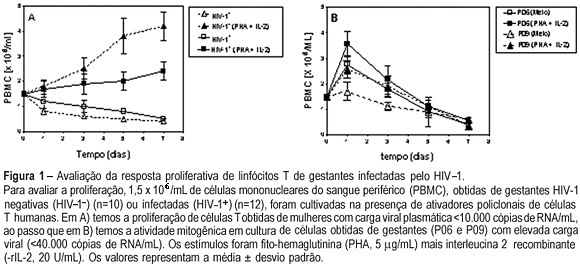
PURPOSE: to evaluate T cell proliferation and cytokine production in HIV-1-infected pregnant women and their impact on in vitro virus replication. METHODS: peripheral blood from 12 HIV-1-infected pregnant women and from their neonates was collected. As control, 10 samples from non-infected pregnants were also colleted. The CD4+ and CD8+ T cell counts were assayed by flow cytometry. Peripheral blood mononuclear cells (PBMC) and plasma were obtained by centrifugation with and without Ficoll-Hypaque gradient, respectively. The freshly purified PBMC were kept in cultures for seven days with PHA plus r-IL-2, and the lymphoproliferative response was assayed by Trypan blue dye exclusion. In some experiments we added anti-IL-10 monoclonal antibody. The plasma samples and supernatants from cell cultures were stored to determine both peripheral cytokine levels, by ELISA sandwich, and viral load, by RT-PCR. RESULTS: the results showed that the lymphoproliferative response was smaller in cultures obtained from HIV-1-infected women than in control cultures [4.2±0.37 vs 2.4±0.56 (x 10(6) cell/mL), p<0.005]. In both control and infected pregnant women who had low plasma viral load, the level of IL-10 was higher than in those with high viral replication (9.790±3.224 vs 1.256±350 pg/mL, p=0.002). The elevated TNF-alpha production detected in serum (7.200±2.440 pg/mL) and supernatants (21.350±15.230 pg/mL) was associated with higher plasma viral loads and vertical infection. The IL-10 blockade by anti-IL-10 antibodies augmented viral replication in the cell cultures. CONCLUSION: these results indicate that IL-10 production exerts a negative influence on virus replication, diminishing the probability of intrauterine HIV-1 infection.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):401-406
DOI 10.1590/S0100-72032005000700006
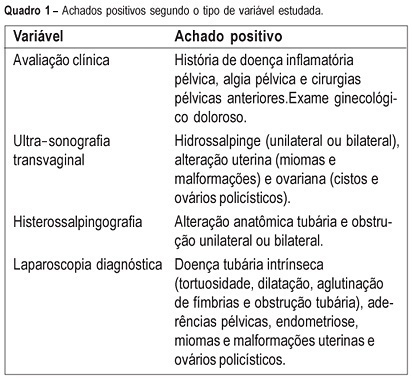
PURPOSE: to evaluate the agreement between noninvasive methods - pelvic pain, transvaginal ultrasound and hysterosalpingography - and the gynecologic endoscopy approach for the diagnosis of tuboperitoneal factors responsible for conjugal infertility. METHODS: this is a cross-sectional study including 149 infertile patients who were submitted to clinical evaluation, transvaginal ultrasound, hysterosalpingography, hysteroscopy, and laparoscopy. In the evaluation of pelvic pain, the following complaints were considered to be abnormal: pelvic pain of the dyspareunia type, dysmenorrhea or acyclic pain, and pain upon mobilization of the cervix and palpation of the adnexa. Ultrasonographic examination was considered to be altered when adnexal or uterine morphological changes (hydrosalpinx, myomas or uterine malformations) were detected. Hysterosalpingography was considered to be abnormal in the presence of anatomical tubal changes and unilateral or bilateral obstruction. The agreement between noninvasive methods and endoscopy was evaluated by kappa statistics. RESULTS: the agreements between pelvic pain, transvaginal ultrasound, and hysterosalpingography and the endoscopic approach were 46.3% (kappa=0.092; CI 95%: -0.043 to 0.228), 24% (kappa=-0.052; CI 95%: -0.148 to 0.043), and 46% (kappa=0.092; CI 95%: -0.043 to 0.228), respectively. When at least one alteration detected by noninvasive methods was considered, the agreement with endoscopic approach was 63% (kappa=-0.014; CI 95%: -0.227 to 0.199). Sensitivity and specificity in predicting alterations on endoscopic approach were 39.5 and 80% in the presence of pelvic pain, 14.5 and 72% in the presence of alteration on transvaginal ultrasound, 39.5 and 80% in the presence of alteration on hysterosalpingography, and 70.2 and 28% in the presence of at least one alteration by noninvasive methods. CONCLUSION: there is a poor diagnostic agreement between the several noninvasive methods and endoscopy in the investigation of conjugal infertility secondary to tuboperitoneal factors.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):425-433
DOI 10.1590/S0100-72032005000700010
Cervical cancer is nowadays a disease amenable to secondary prevention. Methods for the detection of its precursor lesions and human papillomavirus infection, such as cervical cytology and molecular biology, achieved widespread use worldwide. However, there is still too much controversy regarding the use of these methods in gynecological practice. Which is the best examination or the best association of examinations, and the most adequate time intervals to proceed with screening, are still pending questions, generating anxiety in patients and doctors. On the other hand, the management of women who have been diagnosed with viral infection and/or cervical intraepithelial neoplasia is not yet consensual, and several factors may affect the clinical decision on how to treat them. Therapeutic options are dependent upon the type of viral infection, severity of the cervical intraepithelial neoplasia and its histological type. The aim of the present article was to review the several aspects of cervical cancer screening and its viable treatment.