Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):557-562
DOI 10.1590/S0100-72032004000700008
PURPOSE: to determine the prevalence of koilocytosis in penile biopsies of partners of women with HPV-induced genital lesions, and to analyze the risk factors associated with the penile viral infection. METHODS: a total of 80 partners of HPV-infected women with genital lesions were included in this transversal cohort study. The study was carried out between May 2002 and June 2003. The mean age was 34.1 years (16 to 63). No patient reported any kind of genital lesion. They answered questions regarding the presence of urethral symptoms, history of sexually transmitted diseases, number of sexual partners, use of condoms, and circumcision. The patients were submitted to peniscopy with acetic acid and toluidine blue solutions and finally to biopsy of the suspected lesions. Data were analyzed statistically by the chi2 test. RESULTS: the examination was considered negative in 24 patients (30%). All remaining 56 patients (70%) showed white lesions and toluidine blue-positive lesions. Of these, 53 were submitted to biopsy and 41 (77.3%) presented histological changes suggestive of HPV infection. CONCLUSIONS: the prevalence of the male genital infection was 51.2% and no risk factor analyzed was associated with an increased prevalence of HPV genital infection.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):563-571
DOI 10.1590/S0100-72032004000700009
PURPOSE: to measure changes and predictors of changes in mammographic density of climacteric women, before and one year after hormone replacement therapy. METHODS: seventy climacteric women of 45 years or more participated in the study. They were followed-up at a Climacteric Outpatient Service. All of them used regularly either estrogenic or estroprogestative HRT for one year. They were submitted to one basal mammography and another at the end of the first year. HRT schedules could be different from each other, although with the same bioequivalence. Mammographic density was evaluated blindly at the beginning and at the end of the treatment. Age, ovarian function, time since menopause, body mass index, waist/hip ratio, age at menarche, age at first pregnancy, and smoking were evaluated as well. Mammographic density was classified according to the American College of Radiology BI-RADS system into one of the following four parenchymal patterns: A) entirely liposubstituted breasts, B) liposubstituted breasts with disperse glandular parenchyma, C) heterogeneously dense breasts, and D) extremely dense breasts. We proposed a subdivision of each category in to A e A1, B e B1, C and C1, D and D1 in order to identify smaller variations in mammographic density. Therefore, we attributed initial and final scores of 1-8 to each of the patients according to the mammographic density before and after HRT, corresponding to categories A to D1. The proportions of women that presented increase, decrease and no variation in mammographic density after 1 year of HRT were calculated. In addition, we estimated initial to final score variation using the paired t-test of the Statistical Package for Social Sciences (SPSS). RESULTS: mammographic density increased in 22.9%, decreased in 7.1% and did not change in 70% of the studied cases. A significant difference was observed between the score means before (2.2±1.82) and after HRT (2.5±1.9) (p=0.019). The androgenic distribution of body fat was associated with a denser mammographic pattern. CONCLUSIONS: an increase in mammographic density was shown in women undergoing HRT, and was most pronounced in women with androgenic fat distribution. Additional studies must be carried out in order to evaluate if this increment in mammographic density could impair the mammographic screening of breast cancer.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):573-578
DOI 10.1590/S0100-72032004000700010
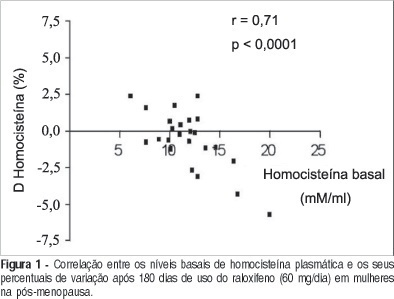
PURPOSE: to evaluate the effects of raloxifene on plasma homocysteine concentration and lipid profile in postmenopausal women. METHODS: twenty-four healthy postmenopausal women, aged 50 to 70 years, with osteopenia and/or osteoporosis, were submitted to raloxifene therapy, 60 mg/day, for six months. Plasma homocysteine concentration was determined before and after three and six months of therapy, as well as total cholesterol, HDL-cholesterol LDL-cholesterol and triglyceride levels. Plasma homocysteine was measured by a polarized immunofluorescence assay and serum lipids by the enzymatic and colorimetric method. Data were analyzed statistically by ANOVA, Newman-Keuls test and Pearson's correlation test. RESULTS: a significant decrease in total cholesterol of 15.3% (227.6±56.3 vs 200.6±29.8 vs 192.8±32.1 mg/dl; p<0.001) and LDL-cholesterol of 21.4% (151.4±46.3 vs 122.7±29.4 vs 119.0±28.6 mg/dl; p<0.001), and a significant increase in HDL-cholesterol of 9.5% (44.7±10.8 vs 52.2±12.6 vs 49.0±10.8 mg/dl; p<0.05) were observed. There was no reduction in triglyceride levels (134.9±50.3 vs 127.5±50.0 vs 121.0±36.0 mg/dl; p>0.05). Although not significant, a decrease in homocysteine by 4.5% (11.7±3.0 vs 11.0±2.9 vs 11.2±2.1 muM/l; p>0.05) was observed between the pre-and posttreatment periods, with a significant negative correlation between basal levels and posttreatment percentual reduction (r=-0.71; p<0.0001). CONCLUSIONS: raloxifene treatment, 60 mg/day, for six months caused a significant decrease in total and LDL-cholesterol and an increase in HDL-cholesterol in postmenopausal women. Plasma homocysteine concentration tended to decrease, this effect being more favorable in patients with elevated baseline levels.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):583-583
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):584-584
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):584-584
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):585-585
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(7):585-585