Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(11):588-592
DOI 10.1590/S0100-72032007001100007
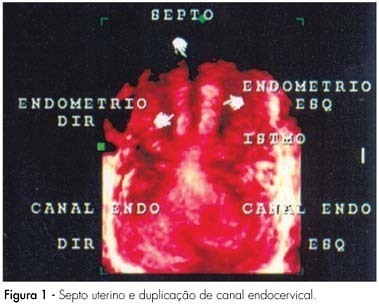
This report describes an unusual case of spontaneous pregnancy in a patient with Müllerian anomaly. The patient was a 34-years old, white, nulligravida, with regular menstrual cycles, and suspected uterine septum observed during a routine ultrasonographic examination. The gynecological examination revealed a complete longitudinal vaginal septum and two uterine cervices. Three-dimensional pelvic ultrasonography showed cervix duplication, uterine septum from isthmus to endometrial cavity and absence of uterine body division, compatible with complete uterine septum and true dual cervices. She returned after one month and reported unprotected sexual intercourse and delayed menstrual period. She was pregnant, had a good pregnancy evolution, and delivered a healthy term baby girl, by cesarean section, at 37 weeks of pregnancy. This report describes a case of normal-term pregnancy in a patient with a rare anomaly (vaginal septum and two cervices) who became spontaneously pregnant without treatment.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(11):593-601
DOI 10.1590/S0100-72032007001100008
There is evidence that estrogen, progesterone and testosterone have modulatory effects over both cellular and humoral immune responses. These effects occur via immune-neuroendocrine interactions, involving the pituitary, gonadal steroids, thymic hormones, and the presence of specific receptors and messengers. These immune responses may be altered during pregnancy, gonadectomy, menopause and hormone therapy. Estrogen depresses the cellular immunity, suppresses the natural killer cell activity and increases the production of antibodies. Progesterone/progestogen suppresses the cellular immune system. Androgens, after metabolization in estrogens, might stimulate the humoral immune response. Hormone therapy is still broadly used in post-menopause women with the purpose of decreasing climacteric symptoms, as well as preventing genital atrophy and bone loss. Its use to attenuate the risk of cardiovascular and neurodegenerative diseases remains in debate. A few studies have been carried out to examine the effect of post-menopause hormone therapy on the immune system. There is evidence that the hypoestrogenic state, following menopause, could result in less resistance to infections. The present review examines the interaction between sexual steroids and the immune system and, based on epidemiological and clinical studies, evaluates the effects of hormone therapy on the immune responses. It was concluded that the hormone therapy normalizes the cellular immune response in post-menopausal women.