Sobre a Revista
A Revista Brasileira de Ginecologia e Obstetrícia (RBGO), publicação de divulgação científica da Federação das Sociedades de Ginecologia e Obstetrícia (FEBRASGO), é dirigida a ginecologistas, obstetras e profissionais de áreas afins, com o objetivo de publicar resultados de pesquisa sobre temas relevantes no campo da Ginecologia, Obstetrícia e áreas correlatas.
- Artigos Recentes
- Mais Citadosi
- Mais Visitadosi
- Artigos Futuros
-
FEBRASGO POSITION STATEMENT16/05/2025
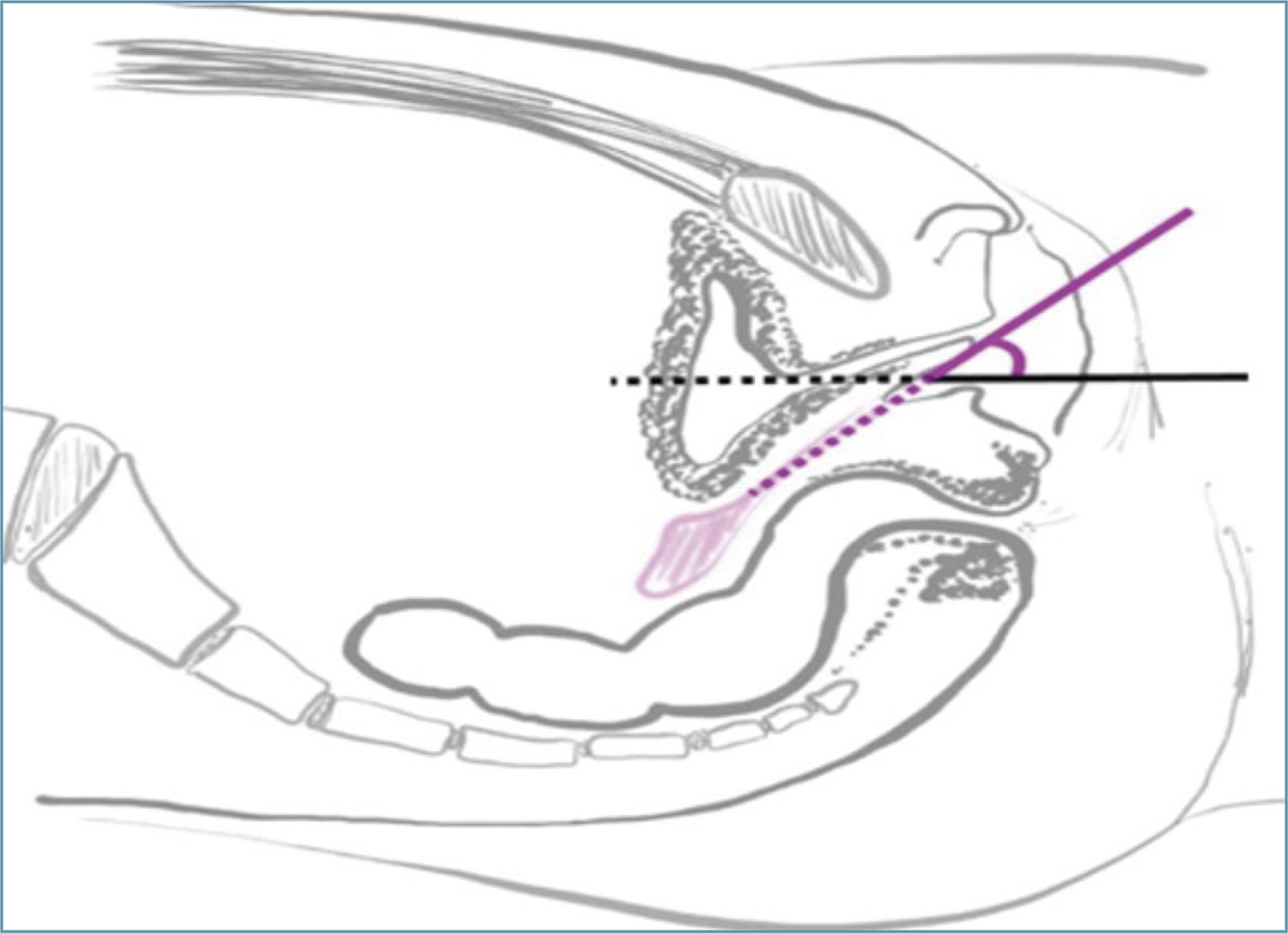
Mayer-Rokitansky-Kuster-Hauser syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-FPS4
Resumo
FEBRASGO POSITION STATEMENTMayer-Rokitansky-Kuster-Hauser syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-FPS4
Visualizações38Ver maisKey points
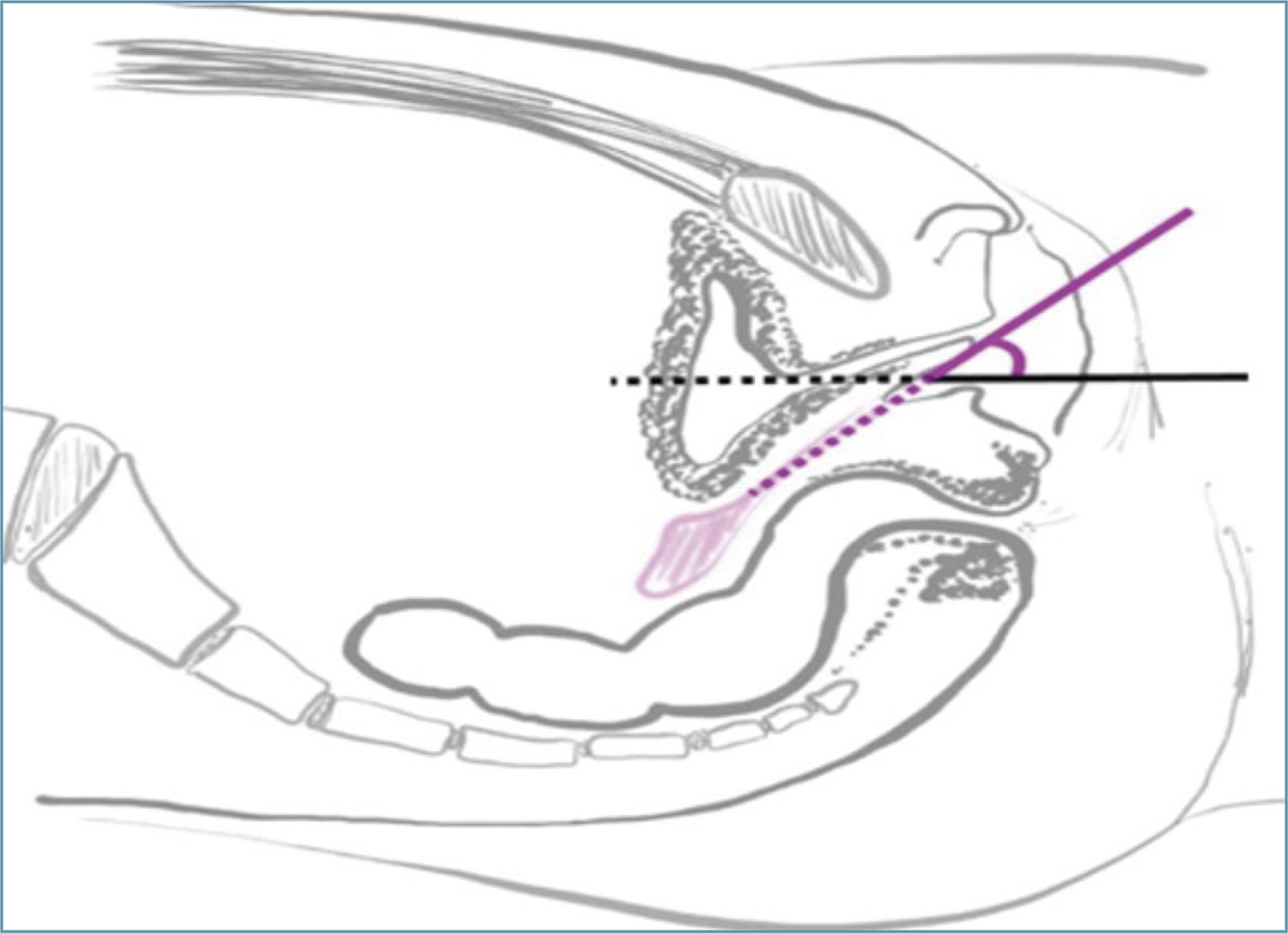
•Mayer-Rokitansky-Kuster-Hauser syndrome (MRKH) is the leading cause of vaginal agenesis.
•It is characterized by primary amenorrhea with typical adrenarche and telarche and may be associated with congenital urological and skeletal conditions that should be investigated.
•Differential diagnoses include: vaginal obstructions (imperforate hymen, distal vaginal atresia, transverse vaginal septum), uterine obstructions (cervical atresia), and differences in sexual development (gonadal dysgenesis, complete androgen insensitivity and congenital adrenal hyperplasia due to CYP17 deficiency).
•Laboratory tests (testosterone, follicle-stimulating hormone [FSH] and karyotype) and radiological tests (pelvic ultrasound and MRI) are necessary.
•Vaginal dilation is the first line of treatment with high success rates.
Visualizações38

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
FEBRASGO POSITION STATEMENTMayer-Rokitansky-Kuster-Hauser syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-FPS4
Visualizações38Ver maisKey points
•Mayer-Rokitansky-Kuster-Hauser syndrome (MRKH) is the leading cause of vaginal agenesis.
•It is characterized by primary amenorrhea with typical adrenarche and telarche and may be associated with congenital urological and skeletal conditions that should be investigated.
•Differential diagnoses include: vaginal obstructions (imperforate hymen, distal vaginal atresia, transverse vaginal septum), uterine obstructions (cervical atresia), and differences in sexual development (gonadal dysgenesis, complete androgen insensitivity and congenital adrenal hyperplasia due to CYP17 deficiency).
•Laboratory tests (testosterone, follicle-stimulating hormone [FSH] and karyotype) and radiological tests (pelvic ultrasound and MRI) are necessary.
•Vaginal dilation is the first line of treatment with high success rates.
-
Original Article30/04/2025
Depression, anxiety, sexual function and quality of life in women with hyperprolactinemia
- Renan Massao Nakamura
 ,
, - Daniela Angerame Yela
 ,
, - Amanda Carvalho Santos
 ,
, - Beatriz Cipriano Ribas
 ,
, - Pedro Henrique Silva Rosa e
 , [ … ],
, [ … ], - Cristina Laguna Benetti-Pinto

Resumo
Original ArticleDepression, anxiety, sexual function and quality of life in women with hyperprolactinemia
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo7
- Renan Massao Nakamura
 ,
, - Daniela Angerame Yela
 ,
, - Amanda Carvalho Santos
 ,
, - Beatriz Cipriano Ribas
 ,
, - Pedro Henrique Silva Rosa e
 ,
, - Bianca Netto Motta
 ,
, - Gabriela Pravatta Rezende
 ,
, - Cristina Laguna Benetti-Pinto

Visualizações49Abstract
Objective:
To evaluate anxiety, depression, sexual function and quality of life in women with hyperprolactinemia.
Methods:
Cross-sectional study with 80 women divided into two groups: 30 women with hyperprolactinemia (Study Group) followed and treated at the endocrine gynecology outpatient clinic and 50 women without hyperprolactinemia, with regular menstrual cycles (Control Group) followed at the family planning outpatient clinic of the State University of Campinas from June 2021 to October 2022. Sociodemographic characteristics, quality of life (SF-36 Questionnaire), sexual function (Female Sexual Function Index Questionnaire), depression (Beck Depression Inventory) and anxiety (Beck Anxiety Scale) were evaluated in both groups. Categorical variables were described as absolute frequency and percentage; numerical variables as mean and standard deviation. Comparison of numerical variables between two groups was performed by Mann-Whitney test, while categorical were compared by Chi-Square or Fisher’s exact tests.
Results:
The mean age of women with hyperprolactinemia was 39.6±8.1 years and the Control Group was 31.2±9.5 years (p<0.001). There was no difference in anxiety scores (p=0.66), depression (p=0.08) and general sexual function (p=0.08) in both groups. However, women with hyperprolactinemia had lower scores in the domains of pain and arousal and worse functional capacity than Control Group (p<0.05).
Conclusion:
Women with hyperprolactinemia under treatment do not show any impairment in their anxiety, depression and sexual function when compared to women without hyperprolactinemia. However, analysis of quality of life showed that women with hyperprolactinemia have poor functional capacity.
Palavras-chave: AnxietyDepressionHyperpituitarismHyperprolactinemiaQuality of lifesexual functionsurveys and questionnairesVer maisVisualizações49

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleDepression, anxiety, sexual function and quality of life in women with hyperprolactinemia
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo7
- Renan Massao Nakamura
 ,
, - Daniela Angerame Yela
 ,
, - Amanda Carvalho Santos
 ,
, - Beatriz Cipriano Ribas
 ,
, - Pedro Henrique Silva Rosa e
 ,
, - Bianca Netto Motta
 ,
, - Gabriela Pravatta Rezende
 ,
, - Cristina Laguna Benetti-Pinto

Visualizações49Abstract
Objective:
To evaluate anxiety, depression, sexual function and quality of life in women with hyperprolactinemia.
Methods:
Cross-sectional study with 80 women divided into two groups: 30 women with hyperprolactinemia (Study Group) followed and treated at the endocrine gynecology outpatient clinic and 50 women without hyperprolactinemia, with regular menstrual cycles (Control Group) followed at the family planning outpatient clinic of the State University of Campinas from June 2021 to October 2022. Sociodemographic characteristics, quality of life (SF-36 Questionnaire), sexual function (Female Sexual Function Index Questionnaire), depression (Beck Depression Inventory) and anxiety (Beck Anxiety Scale) were evaluated in both groups. Categorical variables were described as absolute frequency and percentage; numerical variables as mean and standard deviation. Comparison of numerical variables between two groups was performed by Mann-Whitney test, while categorical were compared by Chi-Square or Fisher’s exact tests.
Results:
The mean age of women with hyperprolactinemia was 39.6±8.1 years and the Control Group was 31.2±9.5 years (p<0.001). There was no difference in anxiety scores (p=0.66), depression (p=0.08) and general sexual function (p=0.08) in both groups. However, women with hyperprolactinemia had lower scores in the domains of pain and arousal and worse functional capacity than Control Group (p<0.05).
Conclusion:
Women with hyperprolactinemia under treatment do not show any impairment in their anxiety, depression and sexual function when compared to women without hyperprolactinemia. However, analysis of quality of life showed that women with hyperprolactinemia have poor functional capacity.
Palavras-chave: AnxietyDepressionHyperpituitarismHyperprolactinemiaQuality of lifesexual functionsurveys and questionnairesVer mais - Renan Massao Nakamura
-
Original Article30/04/2025
Hysterectomy rates per resident in final year of training in teaching hospitals: an ecologic study
- Luiza Nestori Chiozzotto
 ,
, - Nino José Wilson Moterani Júnior
 ,
, - Laura Bresciani Bento Gonçalves Moterani
 ,
, - Vinicius César Moterani
 ,
, - Francisco José Candido dos Reis

Resumo
Original ArticleHysterectomy rates per resident in final year of training in teaching hospitals: an ecologic study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo24
- Luiza Nestori Chiozzotto
 ,
, - Nino José Wilson Moterani Júnior
 ,
, - Laura Bresciani Bento Gonçalves Moterani
 ,
, - Vinicius César Moterani
 ,
, - Francisco José Candido dos Reis

Visualizações92Abstract
Objective:
Analyze the hysterectomy rates per resident in graduation year in teaching hospitals in the state of São Paulo (Brazil).
Methods:
We selected teaching hospitals in the state of São Paulo and gathered information from two public databases to estimate the hysterectomy rates per resident in their final year of training between 2009 and 2019.
Results:
Between 2009 and 2019, there was a 37.5% increase in the number of residents in their final year of training, a 4.31% increase in the number of hysterectomies, and a drop in the hysterectomy rates per resident of 24.1%. The reduction of the rate of hysterectomy per resident was more pronounced for vaginal route (46.4%) followed by abdominal route (23.3%). The ratio of laparoscopic hysterectomy per resident increased 264% during the period, however, this route was used in only 7% of the surgeries in 2019.
Conclusions:
The hysterectomy rates per resident in their final year of training showed a notable reduction. This trend, particularly pronounced in vaginal and abdominal routes, signals a shift towards minimally invasive techniques.
Palavras-chave: Clinical competenceEducation, medicalHospitals, teachingHysterectomylearning curveMedical staff, hospitalPhysiciansStudents, medicalSurgical procedures, operativeVer maisVisualizações92

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleHysterectomy rates per resident in final year of training in teaching hospitals: an ecologic study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo24
- Luiza Nestori Chiozzotto
 ,
, - Nino José Wilson Moterani Júnior
 ,
, - Laura Bresciani Bento Gonçalves Moterani
 ,
, - Vinicius César Moterani
 ,
, - Francisco José Candido dos Reis

Visualizações92Abstract
Objective:
Analyze the hysterectomy rates per resident in graduation year in teaching hospitals in the state of São Paulo (Brazil).
Methods:
We selected teaching hospitals in the state of São Paulo and gathered information from two public databases to estimate the hysterectomy rates per resident in their final year of training between 2009 and 2019.
Results:
Between 2009 and 2019, there was a 37.5% increase in the number of residents in their final year of training, a 4.31% increase in the number of hysterectomies, and a drop in the hysterectomy rates per resident of 24.1%. The reduction of the rate of hysterectomy per resident was more pronounced for vaginal route (46.4%) followed by abdominal route (23.3%). The ratio of laparoscopic hysterectomy per resident increased 264% during the period, however, this route was used in only 7% of the surgeries in 2019.
Conclusions:
The hysterectomy rates per resident in their final year of training showed a notable reduction. This trend, particularly pronounced in vaginal and abdominal routes, signals a shift towards minimally invasive techniques.
Palavras-chave: Clinical competenceEducation, medicalHospitals, teachingHysterectomylearning curveMedical staff, hospitalPhysiciansStudents, medicalSurgical procedures, operativeVer mais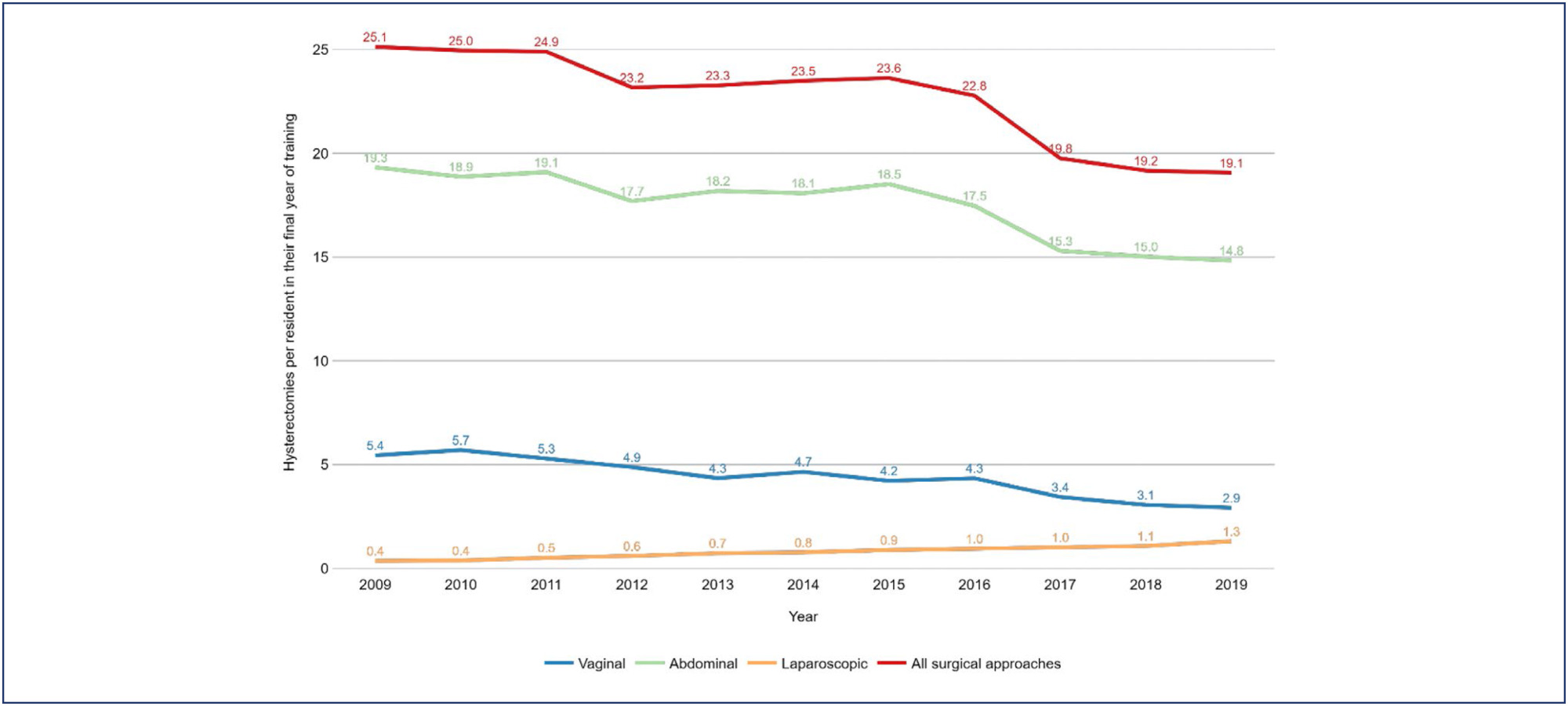
- Luiza Nestori Chiozzotto
-
Original Article30/04/2025
Prevalence of antiphospholipid syndrome among women with recurrent pregnancy loss: a cohort study
- Elaine Cristina Fontes de Oliveira
 ,
, - Daniel Dias Ribeiro
 ,
, - Janaína Campos Senra
 ,
, - Fernando Marcos dos Reis

Resumo
Original ArticlePrevalence of antiphospholipid syndrome among women with recurrent pregnancy loss: a cohort study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo23
- Elaine Cristina Fontes de Oliveira
 ,
, - Daniel Dias Ribeiro
 ,
, - Janaína Campos Senra
 ,
, - Fernando Marcos dos Reis

Visualizações83Abstract
Objective:
This study aimed to evaluate the prevalence of antiphospholipid syndrome (APS) among women experiencing recurrent pregnancy loss (RPL).
Methods:
A cross-sectional was conducted, reviewing the medical records of 134 women with a history of two or more miscarriages, treated between January 2014 and May 2024 at a tertiary university center in Belo Horizonte, Brazil. APS screening was performed by assessing anticardiolipin (IgG and IgM), lupus anticoagulant, and anti-β2-glycoprotein-1 (IgG and IgM) antibodies, based on Sapporo criteria. All tests were performed during non-pregnant periods and at least 12 weeks after the last miscarriage.
Results:
The study included 134 women with a mean age of 33.8 ± 5.7 years. The number of prior miscarriages ranged from 2 to 11 per couple. Among the patients who presented the lupus anticoagulant, only two (1.49%) tested positive in two samples, as per revised Sapporo criteria. Considering IgG and IgM anticardiolipin antibodies, four patients (2.98%) tested positive in two samples according to old Sapporo criteria, with one patient having a positive IgG test in two samples, two having positive IgM in two samples and a single patient having both positive tests. None of the 56 patients tested positive for anti-β2-glycoprotein-1 antibodies in two samples.
Conclusion:
The prevalence of antiphospholipid antibodies, in line with revised Sapporo criteria, is low among Brazilian women with recurrent pregnancy loss, consistent with recent studies in literature. Ensuring the appropriateness of diagnostic criteria is crucial to avoid unnecessary treatment with platelet anticoagulants and heparin in this population.
Palavras-chave: Abortion, habitualAbortion, spontaneousAntibodiesAnticardiolipinAntiphospholipid syndromePrevalenceThrombophiliaVer maisVisualizações83

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticlePrevalence of antiphospholipid syndrome among women with recurrent pregnancy loss: a cohort study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo23
- Elaine Cristina Fontes de Oliveira
 ,
, - Daniel Dias Ribeiro
 ,
, - Janaína Campos Senra
 ,
, - Fernando Marcos dos Reis

Visualizações83Abstract
Objective:
This study aimed to evaluate the prevalence of antiphospholipid syndrome (APS) among women experiencing recurrent pregnancy loss (RPL).
Methods:
A cross-sectional was conducted, reviewing the medical records of 134 women with a history of two or more miscarriages, treated between January 2014 and May 2024 at a tertiary university center in Belo Horizonte, Brazil. APS screening was performed by assessing anticardiolipin (IgG and IgM), lupus anticoagulant, and anti-β2-glycoprotein-1 (IgG and IgM) antibodies, based on Sapporo criteria. All tests were performed during non-pregnant periods and at least 12 weeks after the last miscarriage.
Results:
The study included 134 women with a mean age of 33.8 ± 5.7 years. The number of prior miscarriages ranged from 2 to 11 per couple. Among the patients who presented the lupus anticoagulant, only two (1.49%) tested positive in two samples, as per revised Sapporo criteria. Considering IgG and IgM anticardiolipin antibodies, four patients (2.98%) tested positive in two samples according to old Sapporo criteria, with one patient having a positive IgG test in two samples, two having positive IgM in two samples and a single patient having both positive tests. None of the 56 patients tested positive for anti-β2-glycoprotein-1 antibodies in two samples.
Conclusion:
The prevalence of antiphospholipid antibodies, in line with revised Sapporo criteria, is low among Brazilian women with recurrent pregnancy loss, consistent with recent studies in literature. Ensuring the appropriateness of diagnostic criteria is crucial to avoid unnecessary treatment with platelet anticoagulants and heparin in this population.
Palavras-chave: Abortion, habitualAbortion, spontaneousAntibodiesAnticardiolipinAntiphospholipid syndromePrevalenceThrombophiliaVer mais - Elaine Cristina Fontes de Oliveira
-
Original Article30/04/2025
An assessment of total antioxidant and oxidant parameters and their correlation with embryo quality in in-vitro fertilization patients
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo22
Resumo
Original ArticleAn assessment of total antioxidant and oxidant parameters and their correlation with embryo quality in in-vitro fertilization patients
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo22
Visualizações80Abstract
Objective:
In vitro, fertilization is the primary treatment method for infertility. Follicular fluid analysis is an approach used to optimize the results of assisted reproductive techniques. Oxidative stress represents the imbalance between the production of reactive oxygen species and their detoxification. Total Antioxidant and Oxidant Status, and Oxidative Stress Index levels are the main oxidative stress markers. This study investigated the effects of oxidative stress markers on infertility etiology, embryo quality, and success of In vitro fertilization.
Methods:
Before enrolling in the ICSI-ET cycle, participants had their FSH and LH levels assessed on the second day of the cycle. The ovarian degrees of the participants were evaluated by transvaginal ultrasonography. Participants underwent controlled ovarian stimulation using the GnRH antagonist protocol. TV-USG and serial E2 measurements were performed at appropriate intervals to follow follicular development. Follicle sizes, quantity, and endometrial thickness were recorded. Total Antioxidant and Oxidant Status, and Oxidative analyses were conducted using Rel Assay Diagnostics Assay Kits.
Results:
The average number of total oocytes in the participants was 10.25±6.66, and the average of mature M2 stage oocytes was 6.71±3.72. The average number of fertilized oocytes was 4.65±2.81. Fertilization rates were calculated as approximately 54.75±25.58%. A statistically significant positive correlation was found between embryo quality and serum Total Antioxidant Status levels (p=0.004). Similarly, a significant positive correlation was observed between embryo quality and follicular Total Antioxidant Status values (r = 0.42, p = 0.01).
Conclusion:
This study concluded that oxidative stress markers affect certain stages of the IVF treatment process.
Palavras-chave: AntioxidantsFertilization in vitroFollicular fluidInfertilityOocytesOxidantsOxidative stressVer maisVisualizações80

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleAn assessment of total antioxidant and oxidant parameters and their correlation with embryo quality in in-vitro fertilization patients
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo22
Visualizações80Abstract
Objective:
In vitro, fertilization is the primary treatment method for infertility. Follicular fluid analysis is an approach used to optimize the results of assisted reproductive techniques. Oxidative stress represents the imbalance between the production of reactive oxygen species and their detoxification. Total Antioxidant and Oxidant Status, and Oxidative Stress Index levels are the main oxidative stress markers. This study investigated the effects of oxidative stress markers on infertility etiology, embryo quality, and success of In vitro fertilization.
Methods:
Before enrolling in the ICSI-ET cycle, participants had their FSH and LH levels assessed on the second day of the cycle. The ovarian degrees of the participants were evaluated by transvaginal ultrasonography. Participants underwent controlled ovarian stimulation using the GnRH antagonist protocol. TV-USG and serial E2 measurements were performed at appropriate intervals to follow follicular development. Follicle sizes, quantity, and endometrial thickness were recorded. Total Antioxidant and Oxidant Status, and Oxidative analyses were conducted using Rel Assay Diagnostics Assay Kits.
Results:
The average number of total oocytes in the participants was 10.25±6.66, and the average of mature M2 stage oocytes was 6.71±3.72. The average number of fertilized oocytes was 4.65±2.81. Fertilization rates were calculated as approximately 54.75±25.58%. A statistically significant positive correlation was found between embryo quality and serum Total Antioxidant Status levels (p=0.004). Similarly, a significant positive correlation was observed between embryo quality and follicular Total Antioxidant Status values (r = 0.42, p = 0.01).
Conclusion:
This study concluded that oxidative stress markers affect certain stages of the IVF treatment process.
Palavras-chave: AntioxidantsFertilization in vitroFollicular fluidInfertilityOocytesOxidantsOxidative stressVer mais
-
Review Article30/04/2025
Letrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
- Karine Eskandar
 ,
, - Juliana Almeida Oliveira
 ,
, - Sandro Augusto Ribeiro
 ,
, - Matheus Pedrotti Chavez
 ,
, - Ana Isabela de Araujo Zotti
 , [ … ],
, [ … ], - Andrea Mora de Marco Novellino

Resumo
Review ArticleLetrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
- Karine Eskandar
 ,
, - Juliana Almeida Oliveira
 ,
, - Sandro Augusto Ribeiro
 ,
, - Matheus Pedrotti Chavez
 ,
, - Ana Isabela de Araujo Zotti
 ,
, - Yasmin Jardim Meirelles Dias
 ,
, - Andrea Mora de Marco Novellino

Visualizações93Abstract
Objective:
We aimed to compare the efficacy and safety of letrozole and clomiphene versus letrozole alone for ovulation induction in patients with Polycystic Ovary Syndrome (PCOS).
Data Sources:
We systematically searched EMBASE, PubMed, and Cochrane databases on October 31, 2024.
Study selection:
We included studies of women with PCOS treated with a combination of clomiphene and letrozole or letrozole alone to induce ovulation that reported any of the outcomes of interest, namely rate of mature follicles and ovulation, ovulation, pregnancy, miscarriages, endometrial thickness, and number of mature follicles.
Data collection:
We pooled odds ratios (OR) and mean difference (MD) with 95% confidence intervals (CI) using a random effects model using R statistical software, version 4.2.1. Heterogeneity was assessed with I statistics, and a random effects model was used.
Data Synthesis:
Four RCTs and two observational studies comprising 592 patients were included. Combined therapy was associated with a higher rate of a mature follicle (OR 2.74; 95% CI 1.72-4.37; p< 0.001; I=0%) and ovulation (OR 2.55; 95% CI 1.57-4.12; p< 0.001; I=35.9%). The number of mature follicles, number of pregnancies, thickness of endometrial lining, and the incidence of adverse events, including headache, abdominal bloating, fatigue, back pain, breast discomfort, and night sweats, were similar between groups.
Conclusion:
In women with anovulatory infertility secondary to PCOS, letrozole and clomiphene citrate combined therapy was associated with improved mature follicle and ovulation rates, with a similar safety profile compared to letrozole alone. However, no significant impact was observed on pregnancy rates.
Palavras-chave: ClomipheneInfertility, femaleLetrozoleOvulationOvulation InductionPolycystic ovary syndromeVer maisVisualizações93

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Review ArticleLetrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
- Karine Eskandar
 ,
, - Juliana Almeida Oliveira
 ,
, - Sandro Augusto Ribeiro
 ,
, - Matheus Pedrotti Chavez
 ,
, - Ana Isabela de Araujo Zotti
 ,
, - Yasmin Jardim Meirelles Dias
 ,
, - Andrea Mora de Marco Novellino

Visualizações93Abstract
Objective:
We aimed to compare the efficacy and safety of letrozole and clomiphene versus letrozole alone for ovulation induction in patients with Polycystic Ovary Syndrome (PCOS).
Data Sources:
We systematically searched EMBASE, PubMed, and Cochrane databases on October 31, 2024.
Study selection:
We included studies of women with PCOS treated with a combination of clomiphene and letrozole or letrozole alone to induce ovulation that reported any of the outcomes of interest, namely rate of mature follicles and ovulation, ovulation, pregnancy, miscarriages, endometrial thickness, and number of mature follicles.
Data collection:
We pooled odds ratios (OR) and mean difference (MD) with 95% confidence intervals (CI) using a random effects model using R statistical software, version 4.2.1. Heterogeneity was assessed with I statistics, and a random effects model was used.
Data Synthesis:
Four RCTs and two observational studies comprising 592 patients were included. Combined therapy was associated with a higher rate of a mature follicle (OR 2.74; 95% CI 1.72-4.37; p< 0.001; I=0%) and ovulation (OR 2.55; 95% CI 1.57-4.12; p< 0.001; I=35.9%). The number of mature follicles, number of pregnancies, thickness of endometrial lining, and the incidence of adverse events, including headache, abdominal bloating, fatigue, back pain, breast discomfort, and night sweats, were similar between groups.
Conclusion:
In women with anovulatory infertility secondary to PCOS, letrozole and clomiphene citrate combined therapy was associated with improved mature follicle and ovulation rates, with a similar safety profile compared to letrozole alone. However, no significant impact was observed on pregnancy rates.
Palavras-chave: ClomipheneInfertility, femaleLetrozoleOvulationOvulation InductionPolycystic ovary syndromeVer mais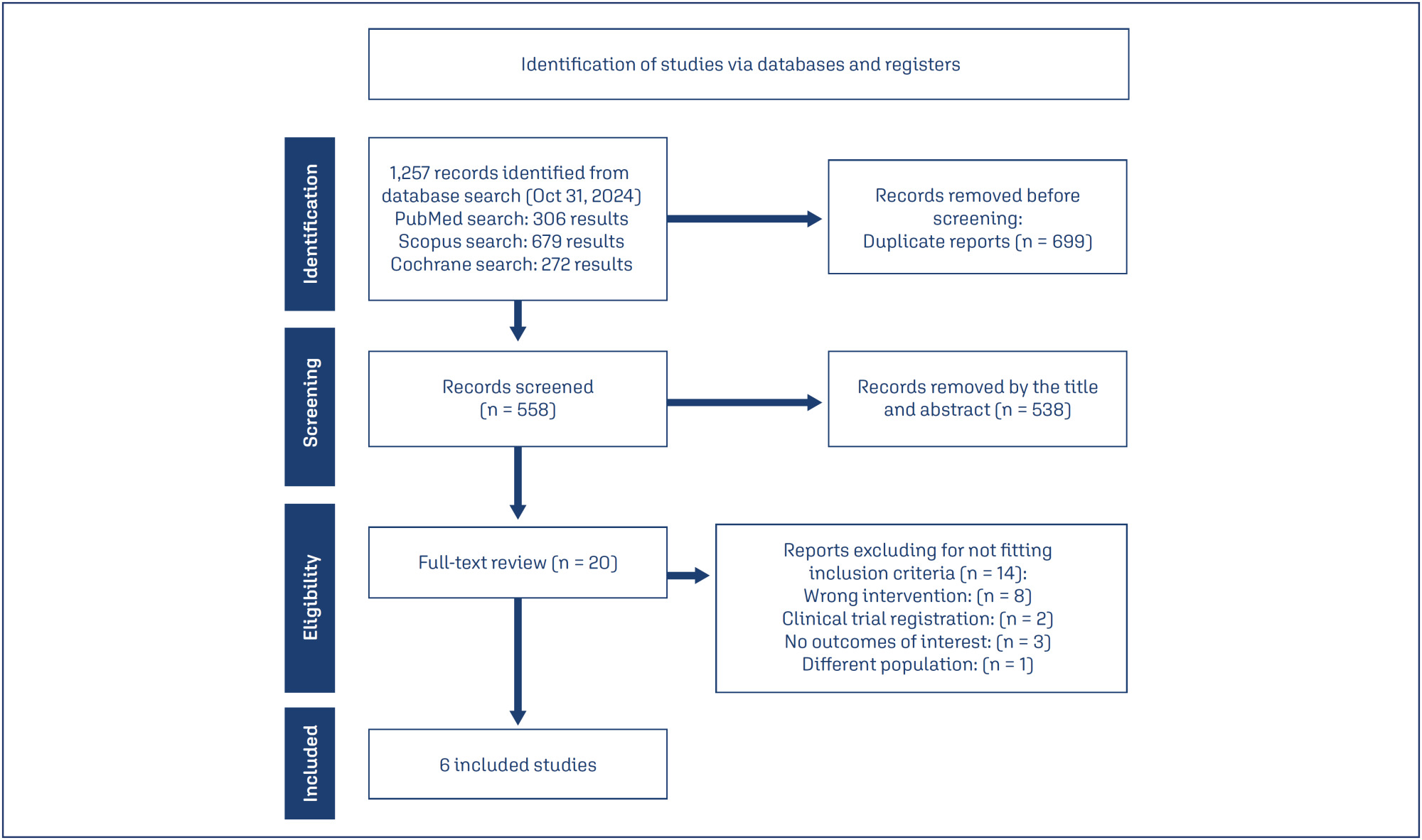
- Karine Eskandar
-
Original Article30/04/2025
Incidence of small-for-gestational-age newborns in pregnant women with COVID-19
- Gustavo dos Santos Raupp
 ,
, - Renato Teixeira Souza
 ,
, - Maria Laura Costa
 ,
, - Jose Guilherme Cecatti
 ,
, - Annerose Barros
 , [ … ],
, [ … ], - Janete Vettorazzi

Resumo
Original ArticleIncidence of small-for-gestational-age newborns in pregnant women with COVID-19
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo20
- Gustavo dos Santos Raupp
 ,
, - Renato Teixeira Souza
 ,
, - Maria Laura Costa
 ,
, - Jose Guilherme Cecatti
 ,
, - Annerose Barros
 ,
, - Ellen Machado Arlindo
 ,
, - Edson Vieira Cunha Filho
 ,
, - Janete Vettorazzi

Visualizações77Abstract
Objective:
This study aimed to assess the incidence of small for gestational age (SGA) newborns in pregnant women infected with COVID-19 and examine the associated neonatal outcomes.
Methods:
This study involved a secondary analysis of the REBRACO Network, a prospective cohort study conducted in 15 maternity hospitals in Brazil before the introduction of COVID-19 vaccination (February 2020 to February 2021). Demographic data of pregnant women tested for COVID-19 were analyzed, and fetal outcomes were compared between women with positive and negative COVID-19 results who had SGA fetuses.
Results:
A total of 729 symptomatic pregnant women with COVID-19 were included in the study. However, there were 248 participants with missing information regarding childbirth or loss of follow-up, and 107 participants without confirmatory tests for COVID-19. Among the remaining participants, 198 had confirmed COVID-19 and 176 tested negative. The incidence of SGA among women with COVID-19 was 22.4%, whereas the incidence among women who tested negative for COVID-19 was 14.8%. SGA newborns born to COVID-19 positive pregnant women were 1.6 times more likely to experience adverse outcomes (such as prematurity, stillbirth, neonatal death, and admission to a neonatal ICU) compared to non-SGA newborns [OR = 1.655 (1.145 – 2.394); P=0.017]. In SGA newborns of pregnant women with confirmed COVID-19 infection, mechanical ventilation use was found to be associated with the infection [OR = 0.692 (0.562 – 0.853); P=0.002].
Conclusion:
The higher incidence of SGA newborns and its stronger association with prematurity in pregnant women with confirmed COVID-19 infection suggest that COVID-19 infection is a significant factor contributing to neonatal morbidity and mortality.
Palavras-chave: coronavirus infectionsCOVID-19Infant, newbornInfant, small for gestational agematernal healthPregnancy complicationsVer maisVisualizações77

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleIncidence of small-for-gestational-age newborns in pregnant women with COVID-19
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo20
- Gustavo dos Santos Raupp
 ,
, - Renato Teixeira Souza
 ,
, - Maria Laura Costa
 ,
, - Jose Guilherme Cecatti
 ,
, - Annerose Barros
 ,
, - Ellen Machado Arlindo
 ,
, - Edson Vieira Cunha Filho
 ,
, - Janete Vettorazzi

Visualizações77Abstract
Objective:
This study aimed to assess the incidence of small for gestational age (SGA) newborns in pregnant women infected with COVID-19 and examine the associated neonatal outcomes.
Methods:
This study involved a secondary analysis of the REBRACO Network, a prospective cohort study conducted in 15 maternity hospitals in Brazil before the introduction of COVID-19 vaccination (February 2020 to February 2021). Demographic data of pregnant women tested for COVID-19 were analyzed, and fetal outcomes were compared between women with positive and negative COVID-19 results who had SGA fetuses.
Results:
A total of 729 symptomatic pregnant women with COVID-19 were included in the study. However, there were 248 participants with missing information regarding childbirth or loss of follow-up, and 107 participants without confirmatory tests for COVID-19. Among the remaining participants, 198 had confirmed COVID-19 and 176 tested negative. The incidence of SGA among women with COVID-19 was 22.4%, whereas the incidence among women who tested negative for COVID-19 was 14.8%. SGA newborns born to COVID-19 positive pregnant women were 1.6 times more likely to experience adverse outcomes (such as prematurity, stillbirth, neonatal death, and admission to a neonatal ICU) compared to non-SGA newborns [OR = 1.655 (1.145 – 2.394); P=0.017]. In SGA newborns of pregnant women with confirmed COVID-19 infection, mechanical ventilation use was found to be associated with the infection [OR = 0.692 (0.562 – 0.853); P=0.002].
Conclusion:
The higher incidence of SGA newborns and its stronger association with prematurity in pregnant women with confirmed COVID-19 infection suggest that COVID-19 infection is a significant factor contributing to neonatal morbidity and mortality.
Palavras-chave: coronavirus infectionsCOVID-19Infant, newbornInfant, small for gestational agematernal healthPregnancy complicationsVer mais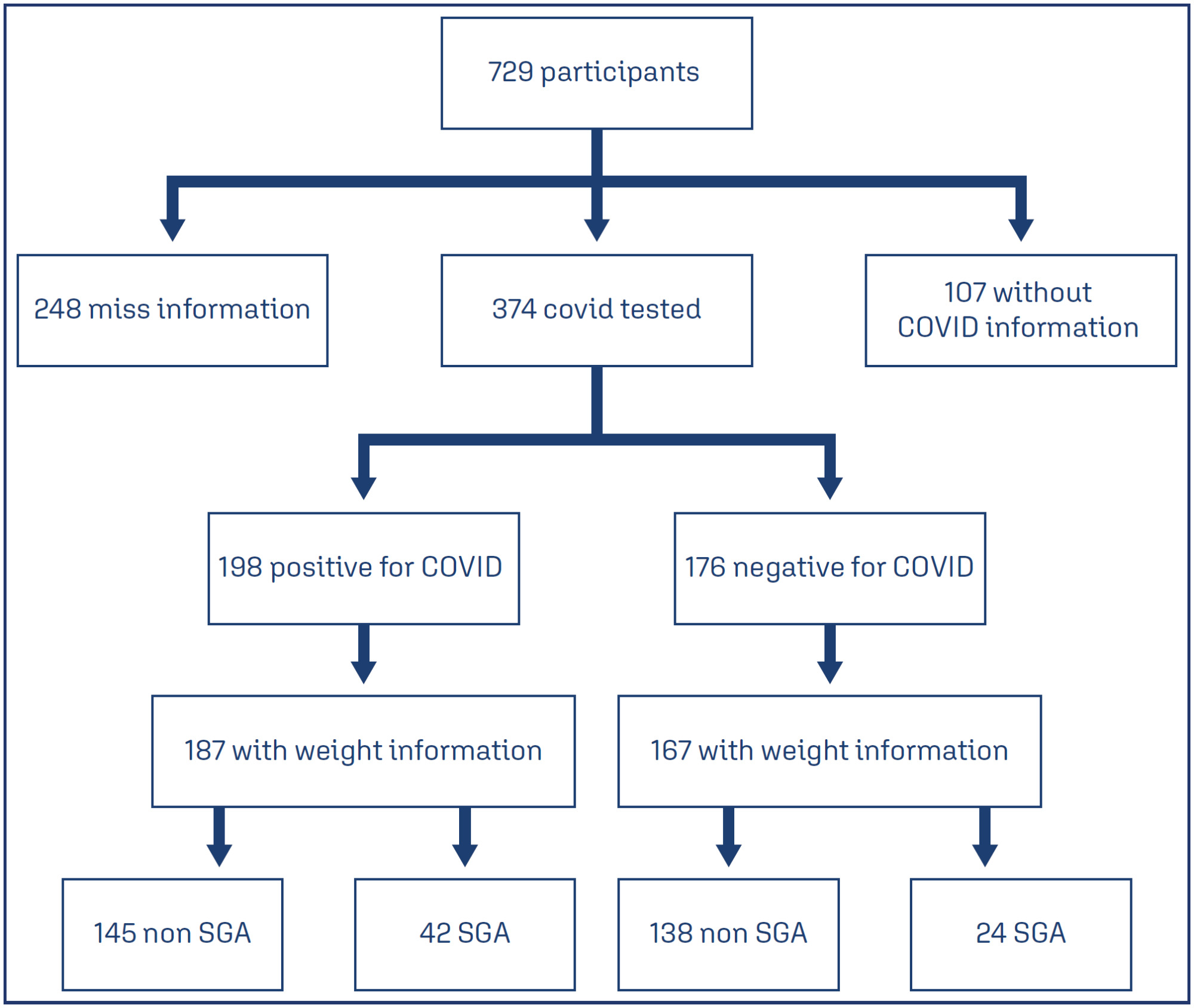
- Gustavo dos Santos Raupp
-
Review Article30/04/2025
Efficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
- Nicole Cristina Lottermann
 ,
, - Nathalia Luiza Andreazza
 ,
, - Matheus de Araújo Moura Cavalcante
 ,
, - Laura Andrade Fernandez
 ,
, - Carla Vitola Gonçalvez
 , [ … ],
, [ … ], - Linjie Zhang

Resumo
Review ArticleEfficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo18
- Nicole Cristina Lottermann
 ,
, - Nathalia Luiza Andreazza
 ,
, - Matheus de Araújo Moura Cavalcante
 ,
, - Laura Andrade Fernandez
 ,
, - Carla Vitola Gonçalvez
 ,
, - Linjie Zhang

Visualizações82Abstract
Objective:
This umbrella review aimed to synthesize evidence from systematic reviews of clinical trials on the efficacy of tranexamic acid in gynecology and obstetrics procedures.
Methods:
We searched Medline, Embase, SciELO and Cochrane Database of Systematic Reviews on March 11, 2024, using the term “tranexamic acid”. Four reviewers independently select studies and extract data. We assessed the quality of systematic review and the quality of evidence, using AMSTAR 2 and GRADE tools, respectively.
Results:
Of 651 systematic reviews identified, 16 reviews with 96663 patients were included. The surgical procedures were cesarean section, myomectomy, hysterectomy, and cervical intraepithelial neoplasia surgery. All reviews showed a statistically significant and clinically relevant reduction in intraoperative and post-procedure blood loss, associated with intravenous or topical use of tranexamic acid. Tranexamic acid resulted in a significant reduction in the need for blood transfusions and a less pronounced drop in postoperative hematocrit and hemoglobin levels in cesarean section. Several reviews addressed the same question, but the number of included trials varied substantially, which might indicate flaws in search and selection of studies of these reviews. The quality of systematic reviews was low or critically low, and the quality of evidence was moderate.
Conclusions:
This umbrella review shows that tranexamic acid can reduce blood loss and hemorrhage in gynecology and obstetrics procedures. High quality systematic reviews are still needed.
Palavras-chave: Blood transfusionCesarean sectionEfficacyGynecologic surgical procedureshematocritHemorrhageHysterectomyObstetric surgical proceduresTranexamic acidUterine cervical dysplasiauterine myomectomyVer maisVisualizações82

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Review ArticleEfficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo18
- Nicole Cristina Lottermann
 ,
, - Nathalia Luiza Andreazza
 ,
, - Matheus de Araújo Moura Cavalcante
 ,
, - Laura Andrade Fernandez
 ,
, - Carla Vitola Gonçalvez
 ,
, - Linjie Zhang

Visualizações82Abstract
Objective:
This umbrella review aimed to synthesize evidence from systematic reviews of clinical trials on the efficacy of tranexamic acid in gynecology and obstetrics procedures.
Methods:
We searched Medline, Embase, SciELO and Cochrane Database of Systematic Reviews on March 11, 2024, using the term “tranexamic acid”. Four reviewers independently select studies and extract data. We assessed the quality of systematic review and the quality of evidence, using AMSTAR 2 and GRADE tools, respectively.
Results:
Of 651 systematic reviews identified, 16 reviews with 96663 patients were included. The surgical procedures were cesarean section, myomectomy, hysterectomy, and cervical intraepithelial neoplasia surgery. All reviews showed a statistically significant and clinically relevant reduction in intraoperative and post-procedure blood loss, associated with intravenous or topical use of tranexamic acid. Tranexamic acid resulted in a significant reduction in the need for blood transfusions and a less pronounced drop in postoperative hematocrit and hemoglobin levels in cesarean section. Several reviews addressed the same question, but the number of included trials varied substantially, which might indicate flaws in search and selection of studies of these reviews. The quality of systematic reviews was low or critically low, and the quality of evidence was moderate.
Conclusions:
This umbrella review shows that tranexamic acid can reduce blood loss and hemorrhage in gynecology and obstetrics procedures. High quality systematic reviews are still needed.
Palavras-chave: Blood transfusionCesarean sectionEfficacyGynecologic surgical procedureshematocritHemorrhageHysterectomyObstetric surgical proceduresTranexamic acidUterine cervical dysplasiauterine myomectomyVer mais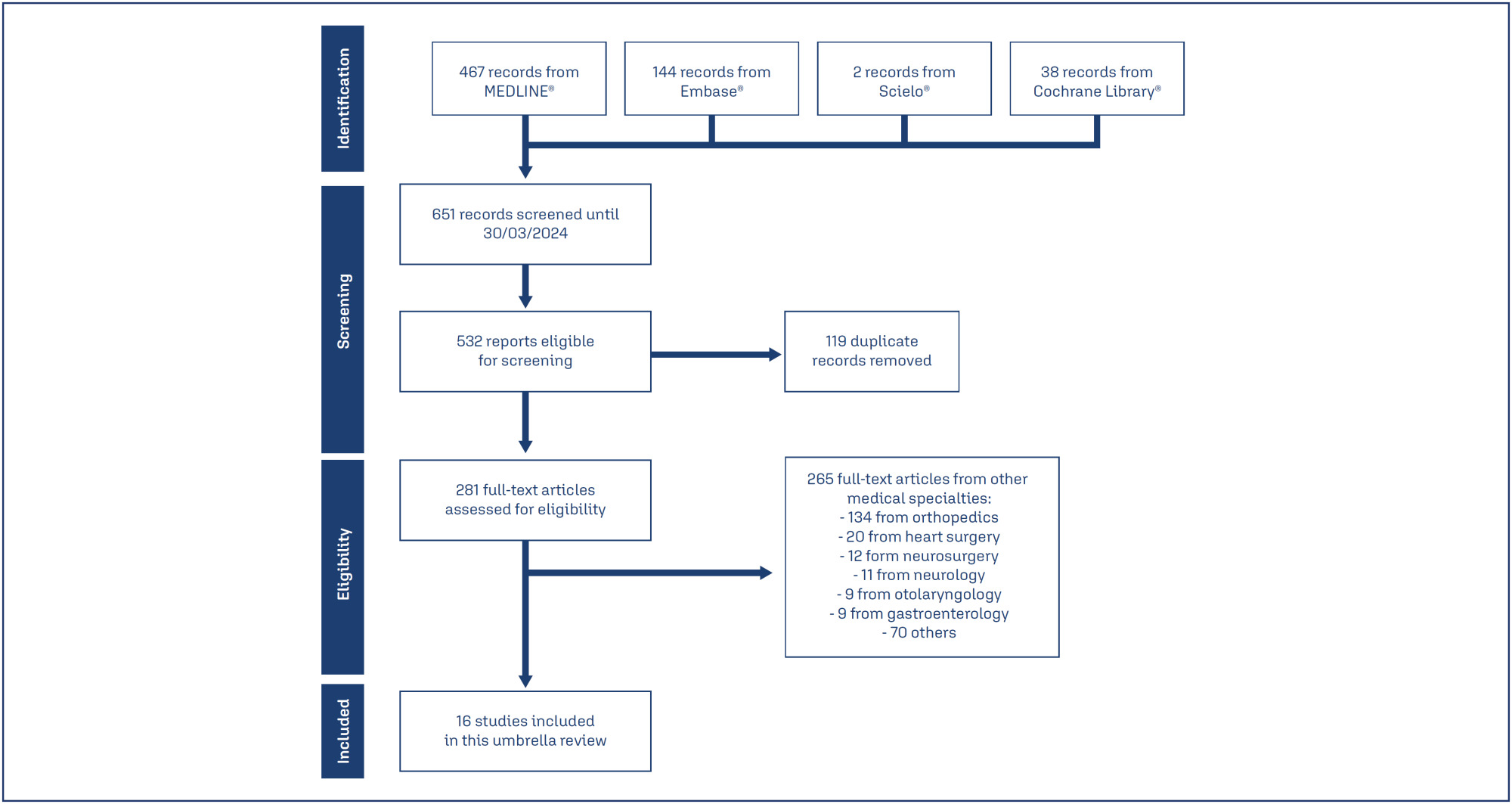
- Nicole Cristina Lottermann
-
FEBRASGO POSITION STATEMENT16/05/2025
Mayer-Rokitansky-Kuster-Hauser syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-FPS4
Resumo
FEBRASGO POSITION STATEMENTMayer-Rokitansky-Kuster-Hauser syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-FPS4
Visualizações38Ver maisKey points
•Mayer-Rokitansky-Kuster-Hauser syndrome (MRKH) is the leading cause of vaginal agenesis.
•It is characterized by primary amenorrhea with typical adrenarche and telarche and may be associated with congenital urological and skeletal conditions that should be investigated.
•Differential diagnoses include: vaginal obstructions (imperforate hymen, distal vaginal atresia, transverse vaginal septum), uterine obstructions (cervical atresia), and differences in sexual development (gonadal dysgenesis, complete androgen insensitivity and congenital adrenal hyperplasia due to CYP17 deficiency).
•Laboratory tests (testosterone, follicle-stimulating hormone [FSH] and karyotype) and radiological tests (pelvic ultrasound and MRI) are necessary.
•Vaginal dilation is the first line of treatment with high success rates.
Visualizações38

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
FEBRASGO POSITION STATEMENTMayer-Rokitansky-Kuster-Hauser syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-FPS4
Visualizações38Ver maisKey points
•Mayer-Rokitansky-Kuster-Hauser syndrome (MRKH) is the leading cause of vaginal agenesis.
•It is characterized by primary amenorrhea with typical adrenarche and telarche and may be associated with congenital urological and skeletal conditions that should be investigated.
•Differential diagnoses include: vaginal obstructions (imperforate hymen, distal vaginal atresia, transverse vaginal septum), uterine obstructions (cervical atresia), and differences in sexual development (gonadal dysgenesis, complete androgen insensitivity and congenital adrenal hyperplasia due to CYP17 deficiency).
•Laboratory tests (testosterone, follicle-stimulating hormone [FSH] and karyotype) and radiological tests (pelvic ultrasound and MRI) are necessary.
•Vaginal dilation is the first line of treatment with high success rates.
-
Original Article30/04/2025
Depression, anxiety, sexual function and quality of life in women with hyperprolactinemia
- Renan Massao Nakamura
 ,
, - Daniela Angerame Yela
 ,
, - Amanda Carvalho Santos
 ,
, - Beatriz Cipriano Ribas
 ,
, - Pedro Henrique Silva Rosa e
 , [ … ],
, [ … ], - Cristina Laguna Benetti-Pinto

Resumo
Original ArticleDepression, anxiety, sexual function and quality of life in women with hyperprolactinemia
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo7
- Renan Massao Nakamura
 ,
, - Daniela Angerame Yela
 ,
, - Amanda Carvalho Santos
 ,
, - Beatriz Cipriano Ribas
 ,
, - Pedro Henrique Silva Rosa e
 ,
, - Bianca Netto Motta
 ,
, - Gabriela Pravatta Rezende
 ,
, - Cristina Laguna Benetti-Pinto

Visualizações49Abstract
Objective:
To evaluate anxiety, depression, sexual function and quality of life in women with hyperprolactinemia.
Methods:
Cross-sectional study with 80 women divided into two groups: 30 women with hyperprolactinemia (Study Group) followed and treated at the endocrine gynecology outpatient clinic and 50 women without hyperprolactinemia, with regular menstrual cycles (Control Group) followed at the family planning outpatient clinic of the State University of Campinas from June 2021 to October 2022. Sociodemographic characteristics, quality of life (SF-36 Questionnaire), sexual function (Female Sexual Function Index Questionnaire), depression (Beck Depression Inventory) and anxiety (Beck Anxiety Scale) were evaluated in both groups. Categorical variables were described as absolute frequency and percentage; numerical variables as mean and standard deviation. Comparison of numerical variables between two groups was performed by Mann-Whitney test, while categorical were compared by Chi-Square or Fisher’s exact tests.
Results:
The mean age of women with hyperprolactinemia was 39.6±8.1 years and the Control Group was 31.2±9.5 years (p<0.001). There was no difference in anxiety scores (p=0.66), depression (p=0.08) and general sexual function (p=0.08) in both groups. However, women with hyperprolactinemia had lower scores in the domains of pain and arousal and worse functional capacity than Control Group (p<0.05).
Conclusion:
Women with hyperprolactinemia under treatment do not show any impairment in their anxiety, depression and sexual function when compared to women without hyperprolactinemia. However, analysis of quality of life showed that women with hyperprolactinemia have poor functional capacity.
Palavras-chave: AnxietyDepressionHyperpituitarismHyperprolactinemiaQuality of lifesexual functionsurveys and questionnairesVer maisVisualizações49

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleDepression, anxiety, sexual function and quality of life in women with hyperprolactinemia
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo7
- Renan Massao Nakamura
 ,
, - Daniela Angerame Yela
 ,
, - Amanda Carvalho Santos
 ,
, - Beatriz Cipriano Ribas
 ,
, - Pedro Henrique Silva Rosa e
 ,
, - Bianca Netto Motta
 ,
, - Gabriela Pravatta Rezende
 ,
, - Cristina Laguna Benetti-Pinto

Visualizações49Abstract
Objective:
To evaluate anxiety, depression, sexual function and quality of life in women with hyperprolactinemia.
Methods:
Cross-sectional study with 80 women divided into two groups: 30 women with hyperprolactinemia (Study Group) followed and treated at the endocrine gynecology outpatient clinic and 50 women without hyperprolactinemia, with regular menstrual cycles (Control Group) followed at the family planning outpatient clinic of the State University of Campinas from June 2021 to October 2022. Sociodemographic characteristics, quality of life (SF-36 Questionnaire), sexual function (Female Sexual Function Index Questionnaire), depression (Beck Depression Inventory) and anxiety (Beck Anxiety Scale) were evaluated in both groups. Categorical variables were described as absolute frequency and percentage; numerical variables as mean and standard deviation. Comparison of numerical variables between two groups was performed by Mann-Whitney test, while categorical were compared by Chi-Square or Fisher’s exact tests.
Results:
The mean age of women with hyperprolactinemia was 39.6±8.1 years and the Control Group was 31.2±9.5 years (p<0.001). There was no difference in anxiety scores (p=0.66), depression (p=0.08) and general sexual function (p=0.08) in both groups. However, women with hyperprolactinemia had lower scores in the domains of pain and arousal and worse functional capacity than Control Group (p<0.05).
Conclusion:
Women with hyperprolactinemia under treatment do not show any impairment in their anxiety, depression and sexual function when compared to women without hyperprolactinemia. However, analysis of quality of life showed that women with hyperprolactinemia have poor functional capacity.
Palavras-chave: AnxietyDepressionHyperpituitarismHyperprolactinemiaQuality of lifesexual functionsurveys and questionnairesVer mais - Renan Massao Nakamura
-
Original Article30/04/2025
Hysterectomy rates per resident in final year of training in teaching hospitals: an ecologic study
- Luiza Nestori Chiozzotto
 ,
, - Nino José Wilson Moterani Júnior
 ,
, - Laura Bresciani Bento Gonçalves Moterani
 ,
, - Vinicius César Moterani
 ,
, - Francisco José Candido dos Reis

Resumo
Original ArticleHysterectomy rates per resident in final year of training in teaching hospitals: an ecologic study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo24
- Luiza Nestori Chiozzotto
 ,
, - Nino José Wilson Moterani Júnior
 ,
, - Laura Bresciani Bento Gonçalves Moterani
 ,
, - Vinicius César Moterani
 ,
, - Francisco José Candido dos Reis

Visualizações92Abstract
Objective:
Analyze the hysterectomy rates per resident in graduation year in teaching hospitals in the state of São Paulo (Brazil).
Methods:
We selected teaching hospitals in the state of São Paulo and gathered information from two public databases to estimate the hysterectomy rates per resident in their final year of training between 2009 and 2019.
Results:
Between 2009 and 2019, there was a 37.5% increase in the number of residents in their final year of training, a 4.31% increase in the number of hysterectomies, and a drop in the hysterectomy rates per resident of 24.1%. The reduction of the rate of hysterectomy per resident was more pronounced for vaginal route (46.4%) followed by abdominal route (23.3%). The ratio of laparoscopic hysterectomy per resident increased 264% during the period, however, this route was used in only 7% of the surgeries in 2019.
Conclusions:
The hysterectomy rates per resident in their final year of training showed a notable reduction. This trend, particularly pronounced in vaginal and abdominal routes, signals a shift towards minimally invasive techniques.
Palavras-chave: Clinical competenceEducation, medicalHospitals, teachingHysterectomylearning curveMedical staff, hospitalPhysiciansStudents, medicalSurgical procedures, operativeVer maisVisualizações92

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleHysterectomy rates per resident in final year of training in teaching hospitals: an ecologic study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo24
- Luiza Nestori Chiozzotto
 ,
, - Nino José Wilson Moterani Júnior
 ,
, - Laura Bresciani Bento Gonçalves Moterani
 ,
, - Vinicius César Moterani
 ,
, - Francisco José Candido dos Reis

Visualizações92Abstract
Objective:
Analyze the hysterectomy rates per resident in graduation year in teaching hospitals in the state of São Paulo (Brazil).
Methods:
We selected teaching hospitals in the state of São Paulo and gathered information from two public databases to estimate the hysterectomy rates per resident in their final year of training between 2009 and 2019.
Results:
Between 2009 and 2019, there was a 37.5% increase in the number of residents in their final year of training, a 4.31% increase in the number of hysterectomies, and a drop in the hysterectomy rates per resident of 24.1%. The reduction of the rate of hysterectomy per resident was more pronounced for vaginal route (46.4%) followed by abdominal route (23.3%). The ratio of laparoscopic hysterectomy per resident increased 264% during the period, however, this route was used in only 7% of the surgeries in 2019.
Conclusions:
The hysterectomy rates per resident in their final year of training showed a notable reduction. This trend, particularly pronounced in vaginal and abdominal routes, signals a shift towards minimally invasive techniques.
Palavras-chave: Clinical competenceEducation, medicalHospitals, teachingHysterectomylearning curveMedical staff, hospitalPhysiciansStudents, medicalSurgical procedures, operativeVer mais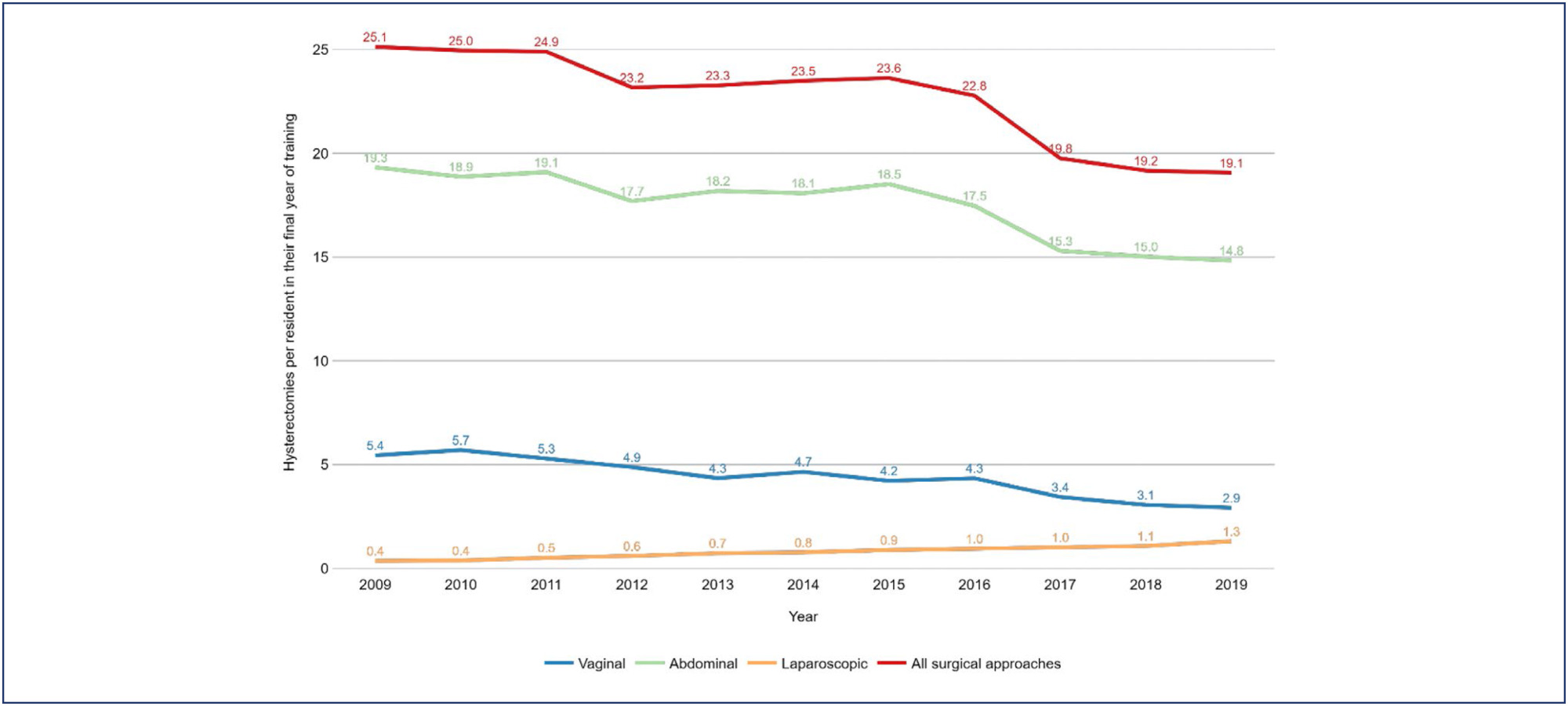
- Luiza Nestori Chiozzotto
-
Original Article30/04/2025
Prevalence of antiphospholipid syndrome among women with recurrent pregnancy loss: a cohort study
- Elaine Cristina Fontes de Oliveira
 ,
, - Daniel Dias Ribeiro
 ,
, - Janaína Campos Senra
 ,
, - Fernando Marcos dos Reis

Resumo
Original ArticlePrevalence of antiphospholipid syndrome among women with recurrent pregnancy loss: a cohort study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo23
- Elaine Cristina Fontes de Oliveira
 ,
, - Daniel Dias Ribeiro
 ,
, - Janaína Campos Senra
 ,
, - Fernando Marcos dos Reis

Visualizações83Abstract
Objective:
This study aimed to evaluate the prevalence of antiphospholipid syndrome (APS) among women experiencing recurrent pregnancy loss (RPL).
Methods:
A cross-sectional was conducted, reviewing the medical records of 134 women with a history of two or more miscarriages, treated between January 2014 and May 2024 at a tertiary university center in Belo Horizonte, Brazil. APS screening was performed by assessing anticardiolipin (IgG and IgM), lupus anticoagulant, and anti-β2-glycoprotein-1 (IgG and IgM) antibodies, based on Sapporo criteria. All tests were performed during non-pregnant periods and at least 12 weeks after the last miscarriage.
Results:
The study included 134 women with a mean age of 33.8 ± 5.7 years. The number of prior miscarriages ranged from 2 to 11 per couple. Among the patients who presented the lupus anticoagulant, only two (1.49%) tested positive in two samples, as per revised Sapporo criteria. Considering IgG and IgM anticardiolipin antibodies, four patients (2.98%) tested positive in two samples according to old Sapporo criteria, with one patient having a positive IgG test in two samples, two having positive IgM in two samples and a single patient having both positive tests. None of the 56 patients tested positive for anti-β2-glycoprotein-1 antibodies in two samples.
Conclusion:
The prevalence of antiphospholipid antibodies, in line with revised Sapporo criteria, is low among Brazilian women with recurrent pregnancy loss, consistent with recent studies in literature. Ensuring the appropriateness of diagnostic criteria is crucial to avoid unnecessary treatment with platelet anticoagulants and heparin in this population.
Palavras-chave: Abortion, habitualAbortion, spontaneousAntibodiesAnticardiolipinAntiphospholipid syndromePrevalenceThrombophiliaVer maisVisualizações83

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticlePrevalence of antiphospholipid syndrome among women with recurrent pregnancy loss: a cohort study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo23
- Elaine Cristina Fontes de Oliveira
 ,
, - Daniel Dias Ribeiro
 ,
, - Janaína Campos Senra
 ,
, - Fernando Marcos dos Reis

Visualizações83Abstract
Objective:
This study aimed to evaluate the prevalence of antiphospholipid syndrome (APS) among women experiencing recurrent pregnancy loss (RPL).
Methods:
A cross-sectional was conducted, reviewing the medical records of 134 women with a history of two or more miscarriages, treated between January 2014 and May 2024 at a tertiary university center in Belo Horizonte, Brazil. APS screening was performed by assessing anticardiolipin (IgG and IgM), lupus anticoagulant, and anti-β2-glycoprotein-1 (IgG and IgM) antibodies, based on Sapporo criteria. All tests were performed during non-pregnant periods and at least 12 weeks after the last miscarriage.
Results:
The study included 134 women with a mean age of 33.8 ± 5.7 years. The number of prior miscarriages ranged from 2 to 11 per couple. Among the patients who presented the lupus anticoagulant, only two (1.49%) tested positive in two samples, as per revised Sapporo criteria. Considering IgG and IgM anticardiolipin antibodies, four patients (2.98%) tested positive in two samples according to old Sapporo criteria, with one patient having a positive IgG test in two samples, two having positive IgM in two samples and a single patient having both positive tests. None of the 56 patients tested positive for anti-β2-glycoprotein-1 antibodies in two samples.
Conclusion:
The prevalence of antiphospholipid antibodies, in line with revised Sapporo criteria, is low among Brazilian women with recurrent pregnancy loss, consistent with recent studies in literature. Ensuring the appropriateness of diagnostic criteria is crucial to avoid unnecessary treatment with platelet anticoagulants and heparin in this population.
Palavras-chave: Abortion, habitualAbortion, spontaneousAntibodiesAnticardiolipinAntiphospholipid syndromePrevalenceThrombophiliaVer mais - Elaine Cristina Fontes de Oliveira
-
Original Article30/04/2025
An assessment of total antioxidant and oxidant parameters and their correlation with embryo quality in in-vitro fertilization patients
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo22
Resumo
Original ArticleAn assessment of total antioxidant and oxidant parameters and their correlation with embryo quality in in-vitro fertilization patients
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo22
Visualizações80Abstract
Objective:
In vitro, fertilization is the primary treatment method for infertility. Follicular fluid analysis is an approach used to optimize the results of assisted reproductive techniques. Oxidative stress represents the imbalance between the production of reactive oxygen species and their detoxification. Total Antioxidant and Oxidant Status, and Oxidative Stress Index levels are the main oxidative stress markers. This study investigated the effects of oxidative stress markers on infertility etiology, embryo quality, and success of In vitro fertilization.
Methods:
Before enrolling in the ICSI-ET cycle, participants had their FSH and LH levels assessed on the second day of the cycle. The ovarian degrees of the participants were evaluated by transvaginal ultrasonography. Participants underwent controlled ovarian stimulation using the GnRH antagonist protocol. TV-USG and serial E2 measurements were performed at appropriate intervals to follow follicular development. Follicle sizes, quantity, and endometrial thickness were recorded. Total Antioxidant and Oxidant Status, and Oxidative analyses were conducted using Rel Assay Diagnostics Assay Kits.
Results:
The average number of total oocytes in the participants was 10.25±6.66, and the average of mature M2 stage oocytes was 6.71±3.72. The average number of fertilized oocytes was 4.65±2.81. Fertilization rates were calculated as approximately 54.75±25.58%. A statistically significant positive correlation was found between embryo quality and serum Total Antioxidant Status levels (p=0.004). Similarly, a significant positive correlation was observed between embryo quality and follicular Total Antioxidant Status values (r = 0.42, p = 0.01).
Conclusion:
This study concluded that oxidative stress markers affect certain stages of the IVF treatment process.
Palavras-chave: AntioxidantsFertilization in vitroFollicular fluidInfertilityOocytesOxidantsOxidative stressVer maisVisualizações80

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleAn assessment of total antioxidant and oxidant parameters and their correlation with embryo quality in in-vitro fertilization patients
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo22
Visualizações80Abstract
Objective:
In vitro, fertilization is the primary treatment method for infertility. Follicular fluid analysis is an approach used to optimize the results of assisted reproductive techniques. Oxidative stress represents the imbalance between the production of reactive oxygen species and their detoxification. Total Antioxidant and Oxidant Status, and Oxidative Stress Index levels are the main oxidative stress markers. This study investigated the effects of oxidative stress markers on infertility etiology, embryo quality, and success of In vitro fertilization.
Methods:
Before enrolling in the ICSI-ET cycle, participants had their FSH and LH levels assessed on the second day of the cycle. The ovarian degrees of the participants were evaluated by transvaginal ultrasonography. Participants underwent controlled ovarian stimulation using the GnRH antagonist protocol. TV-USG and serial E2 measurements were performed at appropriate intervals to follow follicular development. Follicle sizes, quantity, and endometrial thickness were recorded. Total Antioxidant and Oxidant Status, and Oxidative analyses were conducted using Rel Assay Diagnostics Assay Kits.
Results:
The average number of total oocytes in the participants was 10.25±6.66, and the average of mature M2 stage oocytes was 6.71±3.72. The average number of fertilized oocytes was 4.65±2.81. Fertilization rates were calculated as approximately 54.75±25.58%. A statistically significant positive correlation was found between embryo quality and serum Total Antioxidant Status levels (p=0.004). Similarly, a significant positive correlation was observed between embryo quality and follicular Total Antioxidant Status values (r = 0.42, p = 0.01).
Conclusion:
This study concluded that oxidative stress markers affect certain stages of the IVF treatment process.
Palavras-chave: AntioxidantsFertilization in vitroFollicular fluidInfertilityOocytesOxidantsOxidative stressVer mais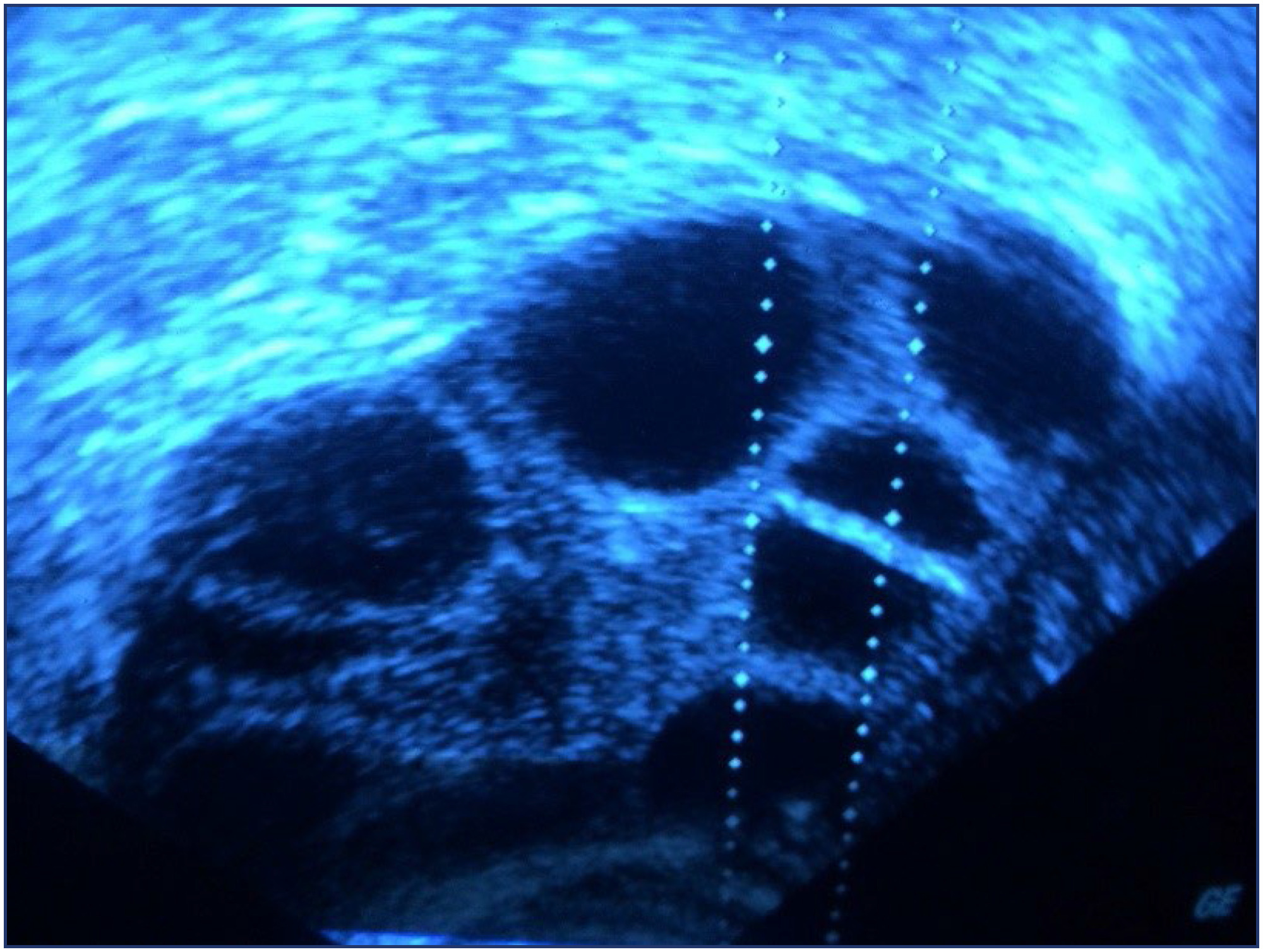
-
Review Article30/04/2025
Letrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
- Karine Eskandar
 ,
, - Juliana Almeida Oliveira
 ,
, - Sandro Augusto Ribeiro
 ,
, - Matheus Pedrotti Chavez
 ,
, - Ana Isabela de Araujo Zotti
 , [ … ],
, [ … ], - Andrea Mora de Marco Novellino

Resumo
Review ArticleLetrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
- Karine Eskandar
 ,
, - Juliana Almeida Oliveira
 ,
, - Sandro Augusto Ribeiro
 ,
, - Matheus Pedrotti Chavez
 ,
, - Ana Isabela de Araujo Zotti
 ,
, - Yasmin Jardim Meirelles Dias
 ,
, - Andrea Mora de Marco Novellino

Visualizações93Abstract
Objective:
We aimed to compare the efficacy and safety of letrozole and clomiphene versus letrozole alone for ovulation induction in patients with Polycystic Ovary Syndrome (PCOS).
Data Sources:
We systematically searched EMBASE, PubMed, and Cochrane databases on October 31, 2024.
Study selection:
We included studies of women with PCOS treated with a combination of clomiphene and letrozole or letrozole alone to induce ovulation that reported any of the outcomes of interest, namely rate of mature follicles and ovulation, ovulation, pregnancy, miscarriages, endometrial thickness, and number of mature follicles.
Data collection:
We pooled odds ratios (OR) and mean difference (MD) with 95% confidence intervals (CI) using a random effects model using R statistical software, version 4.2.1. Heterogeneity was assessed with I statistics, and a random effects model was used.
Data Synthesis:
Four RCTs and two observational studies comprising 592 patients were included. Combined therapy was associated with a higher rate of a mature follicle (OR 2.74; 95% CI 1.72-4.37; p< 0.001; I=0%) and ovulation (OR 2.55; 95% CI 1.57-4.12; p< 0.001; I=35.9%). The number of mature follicles, number of pregnancies, thickness of endometrial lining, and the incidence of adverse events, including headache, abdominal bloating, fatigue, back pain, breast discomfort, and night sweats, were similar between groups.
Conclusion:
In women with anovulatory infertility secondary to PCOS, letrozole and clomiphene citrate combined therapy was associated with improved mature follicle and ovulation rates, with a similar safety profile compared to letrozole alone. However, no significant impact was observed on pregnancy rates.
Palavras-chave: ClomipheneInfertility, femaleLetrozoleOvulationOvulation InductionPolycystic ovary syndromeVer maisVisualizações93

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Review ArticleLetrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
- Karine Eskandar
 ,
, - Juliana Almeida Oliveira
 ,
, - Sandro Augusto Ribeiro
 ,
, - Matheus Pedrotti Chavez
 ,
, - Ana Isabela de Araujo Zotti
 ,
, - Yasmin Jardim Meirelles Dias
 ,
, - Andrea Mora de Marco Novellino

Visualizações93Abstract
Objective:
We aimed to compare the efficacy and safety of letrozole and clomiphene versus letrozole alone for ovulation induction in patients with Polycystic Ovary Syndrome (PCOS).
Data Sources:
We systematically searched EMBASE, PubMed, and Cochrane databases on October 31, 2024.
Study selection:
We included studies of women with PCOS treated with a combination of clomiphene and letrozole or letrozole alone to induce ovulation that reported any of the outcomes of interest, namely rate of mature follicles and ovulation, ovulation, pregnancy, miscarriages, endometrial thickness, and number of mature follicles.
Data collection:
We pooled odds ratios (OR) and mean difference (MD) with 95% confidence intervals (CI) using a random effects model using R statistical software, version 4.2.1. Heterogeneity was assessed with I statistics, and a random effects model was used.
Data Synthesis:
Four RCTs and two observational studies comprising 592 patients were included. Combined therapy was associated with a higher rate of a mature follicle (OR 2.74; 95% CI 1.72-4.37; p< 0.001; I=0%) and ovulation (OR 2.55; 95% CI 1.57-4.12; p< 0.001; I=35.9%). The number of mature follicles, number of pregnancies, thickness of endometrial lining, and the incidence of adverse events, including headache, abdominal bloating, fatigue, back pain, breast discomfort, and night sweats, were similar between groups.
Conclusion:
In women with anovulatory infertility secondary to PCOS, letrozole and clomiphene citrate combined therapy was associated with improved mature follicle and ovulation rates, with a similar safety profile compared to letrozole alone. However, no significant impact was observed on pregnancy rates.
Palavras-chave: ClomipheneInfertility, femaleLetrozoleOvulationOvulation InductionPolycystic ovary syndromeVer mais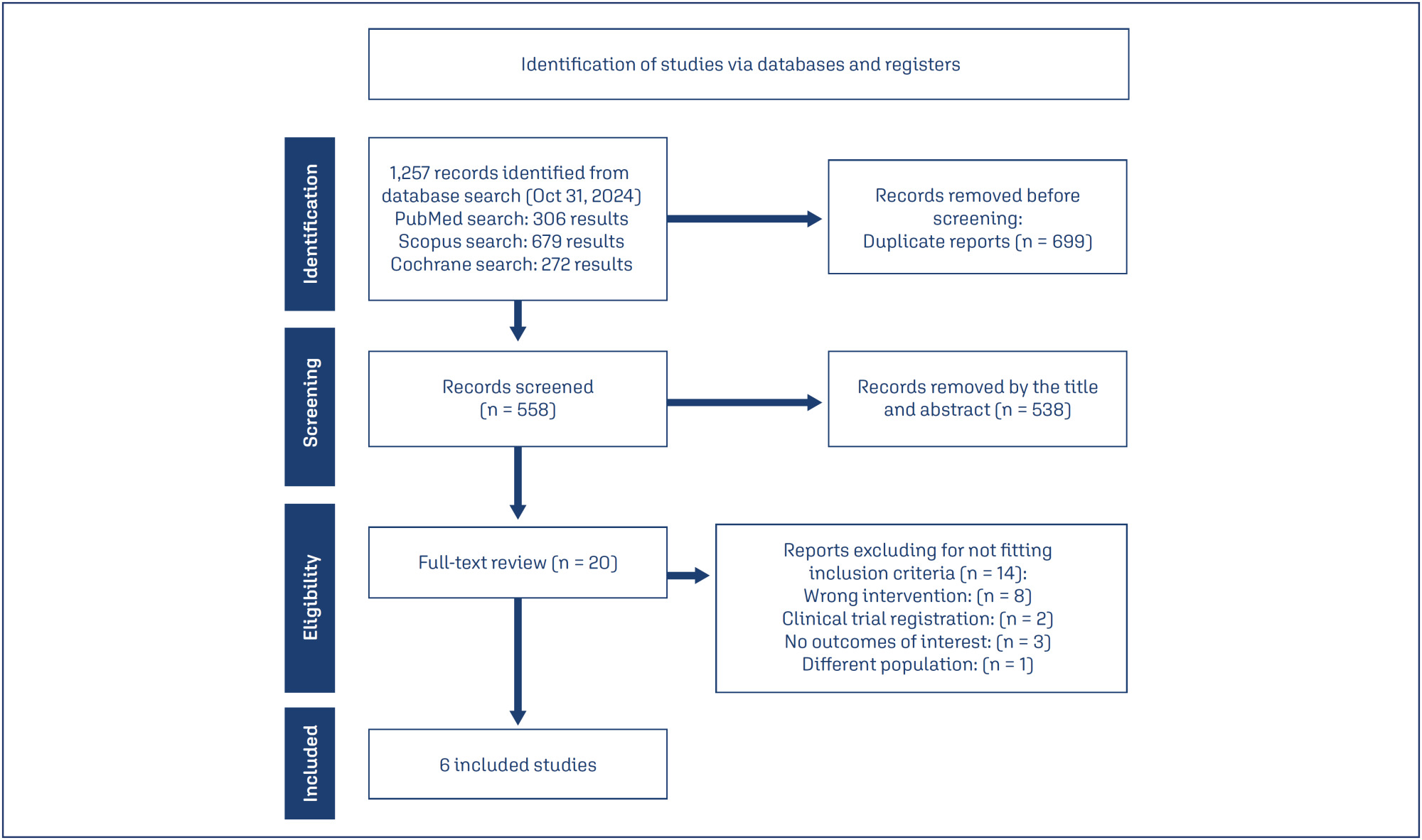
- Karine Eskandar
-
Original Article30/04/2025
Incidence of small-for-gestational-age newborns in pregnant women with COVID-19
- Gustavo dos Santos Raupp
 ,
, - Renato Teixeira Souza
 ,
, - Maria Laura Costa
 ,
, - Jose Guilherme Cecatti
 ,
, - Annerose Barros
 , [ … ],
, [ … ], - Janete Vettorazzi

Resumo
Original ArticleIncidence of small-for-gestational-age newborns in pregnant women with COVID-19
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo20
- Gustavo dos Santos Raupp
 ,
, - Renato Teixeira Souza
 ,
, - Maria Laura Costa
 ,
, - Jose Guilherme Cecatti
 ,
, - Annerose Barros
 ,
, - Ellen Machado Arlindo
 ,
, - Edson Vieira Cunha Filho
 ,
, - Janete Vettorazzi

Visualizações77Abstract
Objective:
This study aimed to assess the incidence of small for gestational age (SGA) newborns in pregnant women infected with COVID-19 and examine the associated neonatal outcomes.
Methods:
This study involved a secondary analysis of the REBRACO Network, a prospective cohort study conducted in 15 maternity hospitals in Brazil before the introduction of COVID-19 vaccination (February 2020 to February 2021). Demographic data of pregnant women tested for COVID-19 were analyzed, and fetal outcomes were compared between women with positive and negative COVID-19 results who had SGA fetuses.
Results:
A total of 729 symptomatic pregnant women with COVID-19 were included in the study. However, there were 248 participants with missing information regarding childbirth or loss of follow-up, and 107 participants without confirmatory tests for COVID-19. Among the remaining participants, 198 had confirmed COVID-19 and 176 tested negative. The incidence of SGA among women with COVID-19 was 22.4%, whereas the incidence among women who tested negative for COVID-19 was 14.8%. SGA newborns born to COVID-19 positive pregnant women were 1.6 times more likely to experience adverse outcomes (such as prematurity, stillbirth, neonatal death, and admission to a neonatal ICU) compared to non-SGA newborns [OR = 1.655 (1.145 – 2.394); P=0.017]. In SGA newborns of pregnant women with confirmed COVID-19 infection, mechanical ventilation use was found to be associated with the infection [OR = 0.692 (0.562 – 0.853); P=0.002].
Conclusion:
The higher incidence of SGA newborns and its stronger association with prematurity in pregnant women with confirmed COVID-19 infection suggest that COVID-19 infection is a significant factor contributing to neonatal morbidity and mortality.
Palavras-chave: coronavirus infectionsCOVID-19Infant, newbornInfant, small for gestational agematernal healthPregnancy complicationsVer maisVisualizações77

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleIncidence of small-for-gestational-age newborns in pregnant women with COVID-19
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo20
- Gustavo dos Santos Raupp
 ,
, - Renato Teixeira Souza
 ,
, - Maria Laura Costa
 ,
, - Jose Guilherme Cecatti
 ,
, - Annerose Barros
 ,
, - Ellen Machado Arlindo
 ,
, - Edson Vieira Cunha Filho
 ,
, - Janete Vettorazzi

Visualizações77Abstract
Objective:
This study aimed to assess the incidence of small for gestational age (SGA) newborns in pregnant women infected with COVID-19 and examine the associated neonatal outcomes.
Methods:
This study involved a secondary analysis of the REBRACO Network, a prospective cohort study conducted in 15 maternity hospitals in Brazil before the introduction of COVID-19 vaccination (February 2020 to February 2021). Demographic data of pregnant women tested for COVID-19 were analyzed, and fetal outcomes were compared between women with positive and negative COVID-19 results who had SGA fetuses.
Results:
A total of 729 symptomatic pregnant women with COVID-19 were included in the study. However, there were 248 participants with missing information regarding childbirth or loss of follow-up, and 107 participants without confirmatory tests for COVID-19. Among the remaining participants, 198 had confirmed COVID-19 and 176 tested negative. The incidence of SGA among women with COVID-19 was 22.4%, whereas the incidence among women who tested negative for COVID-19 was 14.8%. SGA newborns born to COVID-19 positive pregnant women were 1.6 times more likely to experience adverse outcomes (such as prematurity, stillbirth, neonatal death, and admission to a neonatal ICU) compared to non-SGA newborns [OR = 1.655 (1.145 – 2.394); P=0.017]. In SGA newborns of pregnant women with confirmed COVID-19 infection, mechanical ventilation use was found to be associated with the infection [OR = 0.692 (0.562 – 0.853); P=0.002].
Conclusion:
The higher incidence of SGA newborns and its stronger association with prematurity in pregnant women with confirmed COVID-19 infection suggest that COVID-19 infection is a significant factor contributing to neonatal morbidity and mortality.
Palavras-chave: coronavirus infectionsCOVID-19Infant, newbornInfant, small for gestational agematernal healthPregnancy complicationsVer mais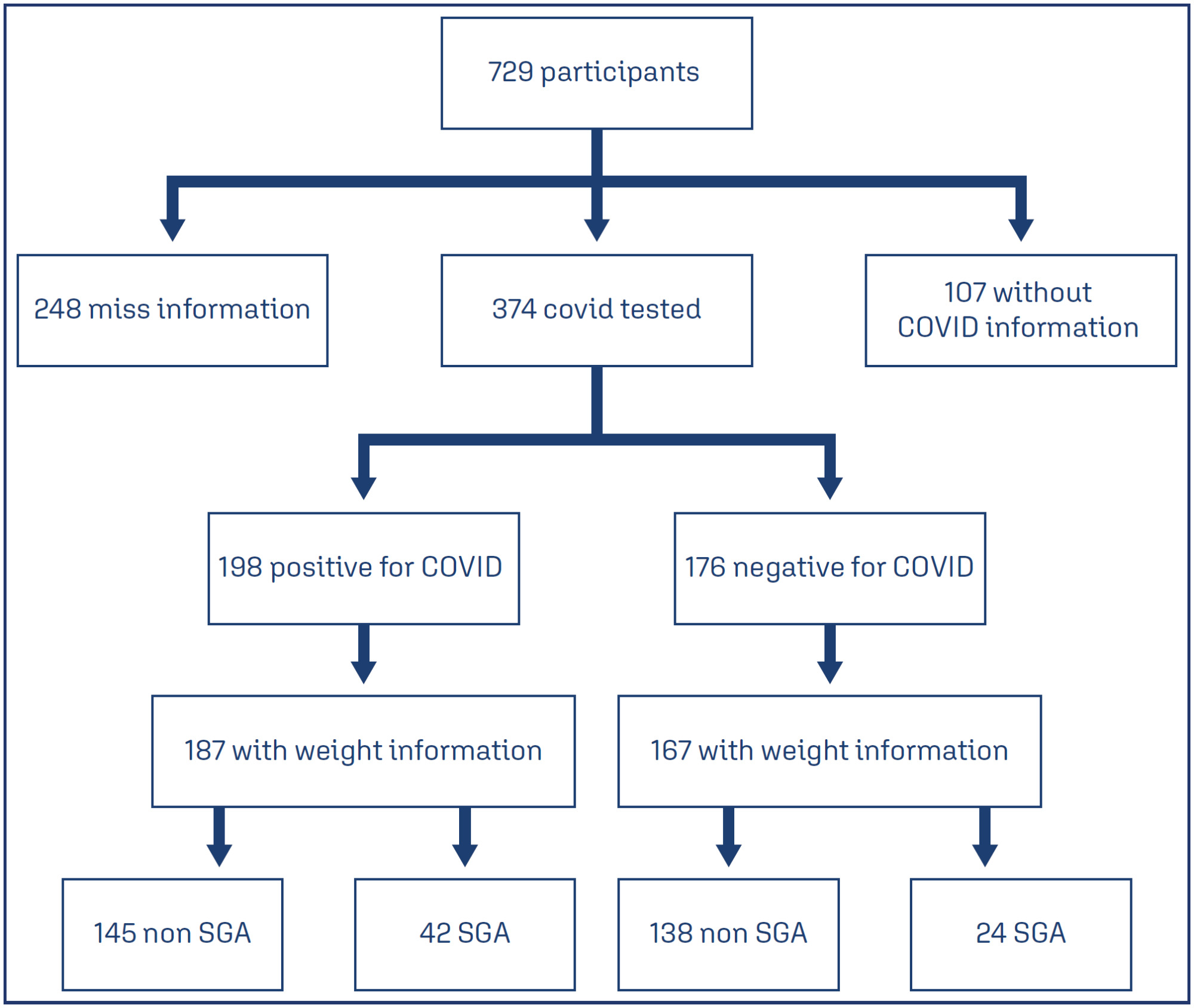
- Gustavo dos Santos Raupp
-
Review Article30/04/2025
Efficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
- Nicole Cristina Lottermann
 ,
, - Nathalia Luiza Andreazza
 ,
, - Matheus de Araújo Moura Cavalcante
 ,
, - Laura Andrade Fernandez
 ,
, - Carla Vitola Gonçalvez
 , [ … ],
, [ … ], - Linjie Zhang

Resumo
Review ArticleEfficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo18
- Nicole Cristina Lottermann
 ,
, - Nathalia Luiza Andreazza
 ,
, - Matheus de Araújo Moura Cavalcante
 ,
, - Laura Andrade Fernandez
 ,
, - Carla Vitola Gonçalvez
 ,
, - Linjie Zhang

Visualizações82Abstract
Objective:
This umbrella review aimed to synthesize evidence from systematic reviews of clinical trials on the efficacy of tranexamic acid in gynecology and obstetrics procedures.
Methods:
We searched Medline, Embase, SciELO and Cochrane Database of Systematic Reviews on March 11, 2024, using the term “tranexamic acid”. Four reviewers independently select studies and extract data. We assessed the quality of systematic review and the quality of evidence, using AMSTAR 2 and GRADE tools, respectively.
Results:
Of 651 systematic reviews identified, 16 reviews with 96663 patients were included. The surgical procedures were cesarean section, myomectomy, hysterectomy, and cervical intraepithelial neoplasia surgery. All reviews showed a statistically significant and clinically relevant reduction in intraoperative and post-procedure blood loss, associated with intravenous or topical use of tranexamic acid. Tranexamic acid resulted in a significant reduction in the need for blood transfusions and a less pronounced drop in postoperative hematocrit and hemoglobin levels in cesarean section. Several reviews addressed the same question, but the number of included trials varied substantially, which might indicate flaws in search and selection of studies of these reviews. The quality of systematic reviews was low or critically low, and the quality of evidence was moderate.
Conclusions:
This umbrella review shows that tranexamic acid can reduce blood loss and hemorrhage in gynecology and obstetrics procedures. High quality systematic reviews are still needed.
Palavras-chave: Blood transfusionCesarean sectionEfficacyGynecologic surgical procedureshematocritHemorrhageHysterectomyObstetric surgical proceduresTranexamic acidUterine cervical dysplasiauterine myomectomyVer maisVisualizações82

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Review ArticleEfficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo18
- Nicole Cristina Lottermann
 ,
, - Nathalia Luiza Andreazza
 ,
, - Matheus de Araújo Moura Cavalcante
 ,
, - Laura Andrade Fernandez
 ,
, - Carla Vitola Gonçalvez
 ,
, - Linjie Zhang

Visualizações82Abstract
Objective:
This umbrella review aimed to synthesize evidence from systematic reviews of clinical trials on the efficacy of tranexamic acid in gynecology and obstetrics procedures.
Methods:
We searched Medline, Embase, SciELO and Cochrane Database of Systematic Reviews on March 11, 2024, using the term “tranexamic acid”. Four reviewers independently select studies and extract data. We assessed the quality of systematic review and the quality of evidence, using AMSTAR 2 and GRADE tools, respectively.
Results:
Of 651 systematic reviews identified, 16 reviews with 96663 patients were included. The surgical procedures were cesarean section, myomectomy, hysterectomy, and cervical intraepithelial neoplasia surgery. All reviews showed a statistically significant and clinically relevant reduction in intraoperative and post-procedure blood loss, associated with intravenous or topical use of tranexamic acid. Tranexamic acid resulted in a significant reduction in the need for blood transfusions and a less pronounced drop in postoperative hematocrit and hemoglobin levels in cesarean section. Several reviews addressed the same question, but the number of included trials varied substantially, which might indicate flaws in search and selection of studies of these reviews. The quality of systematic reviews was low or critically low, and the quality of evidence was moderate.
Conclusions:
This umbrella review shows that tranexamic acid can reduce blood loss and hemorrhage in gynecology and obstetrics procedures. High quality systematic reviews are still needed.
Palavras-chave: Blood transfusionCesarean sectionEfficacyGynecologic surgical procedureshematocritHemorrhageHysterectomyObstetric surgical proceduresTranexamic acidUterine cervical dysplasiauterine myomectomyVer mais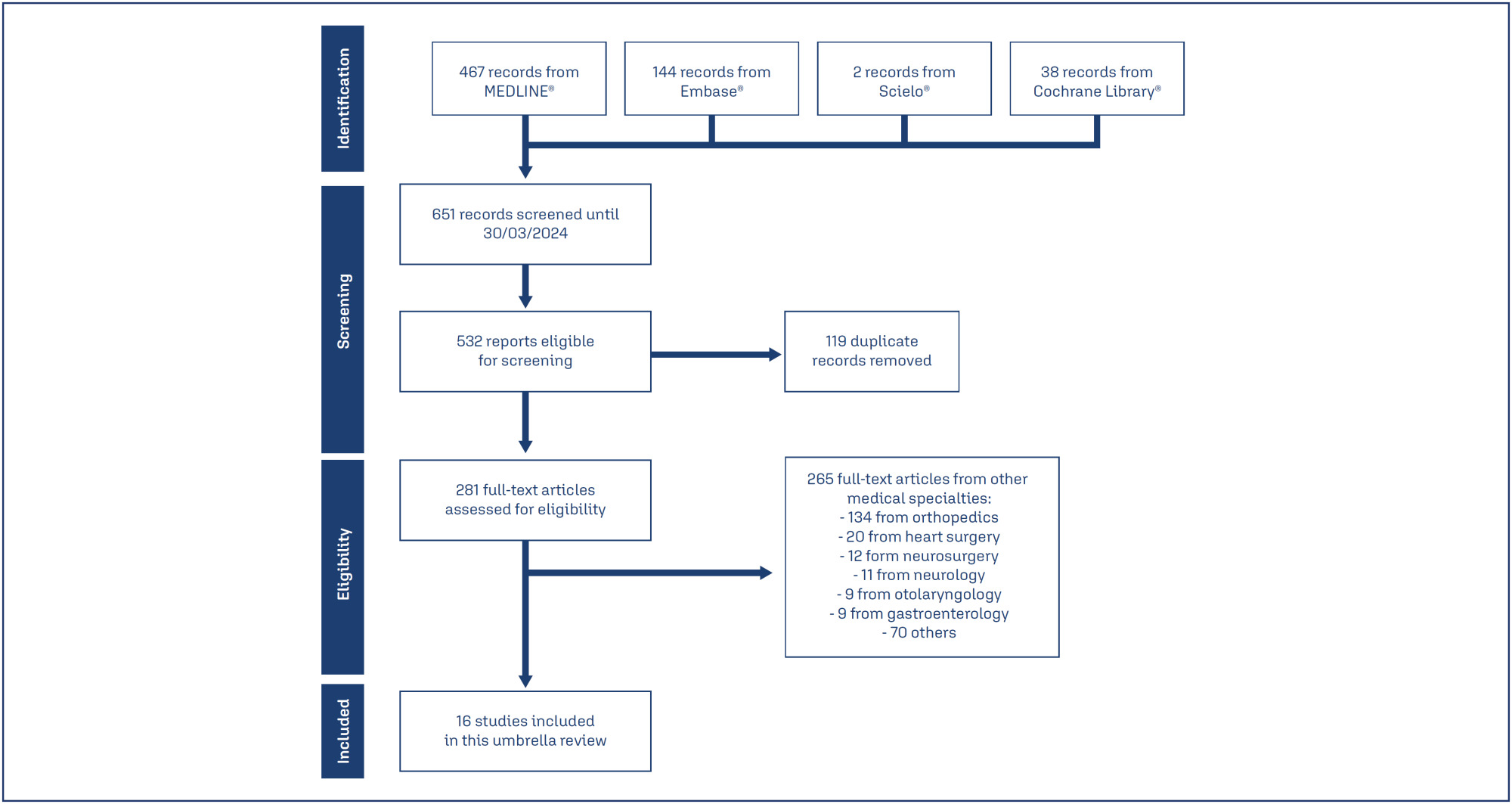
- Nicole Cristina Lottermann
-
FEBRASGO POSITION STATEMENT16/05/2025
Mayer-Rokitansky-Kuster-Hauser syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-FPS4
Resumo
FEBRASGO POSITION STATEMENTMayer-Rokitansky-Kuster-Hauser syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-FPS4
Visualizações38Ver maisKey points
•Mayer-Rokitansky-Kuster-Hauser syndrome (MRKH) is the leading cause of vaginal agenesis.
•It is characterized by primary amenorrhea with typical adrenarche and telarche and may be associated with congenital urological and skeletal conditions that should be investigated.
•Differential diagnoses include: vaginal obstructions (imperforate hymen, distal vaginal atresia, transverse vaginal septum), uterine obstructions (cervical atresia), and differences in sexual development (gonadal dysgenesis, complete androgen insensitivity and congenital adrenal hyperplasia due to CYP17 deficiency).
•Laboratory tests (testosterone, follicle-stimulating hormone [FSH] and karyotype) and radiological tests (pelvic ultrasound and MRI) are necessary.
•Vaginal dilation is the first line of treatment with high success rates.
Visualizações38

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
FEBRASGO POSITION STATEMENTMayer-Rokitansky-Kuster-Hauser syndrome
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-FPS4
Visualizações38Ver maisKey points
•Mayer-Rokitansky-Kuster-Hauser syndrome (MRKH) is the leading cause of vaginal agenesis.
•It is characterized by primary amenorrhea with typical adrenarche and telarche and may be associated with congenital urological and skeletal conditions that should be investigated.
•Differential diagnoses include: vaginal obstructions (imperforate hymen, distal vaginal atresia, transverse vaginal septum), uterine obstructions (cervical atresia), and differences in sexual development (gonadal dysgenesis, complete androgen insensitivity and congenital adrenal hyperplasia due to CYP17 deficiency).
•Laboratory tests (testosterone, follicle-stimulating hormone [FSH] and karyotype) and radiological tests (pelvic ultrasound and MRI) are necessary.
•Vaginal dilation is the first line of treatment with high success rates.


This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. 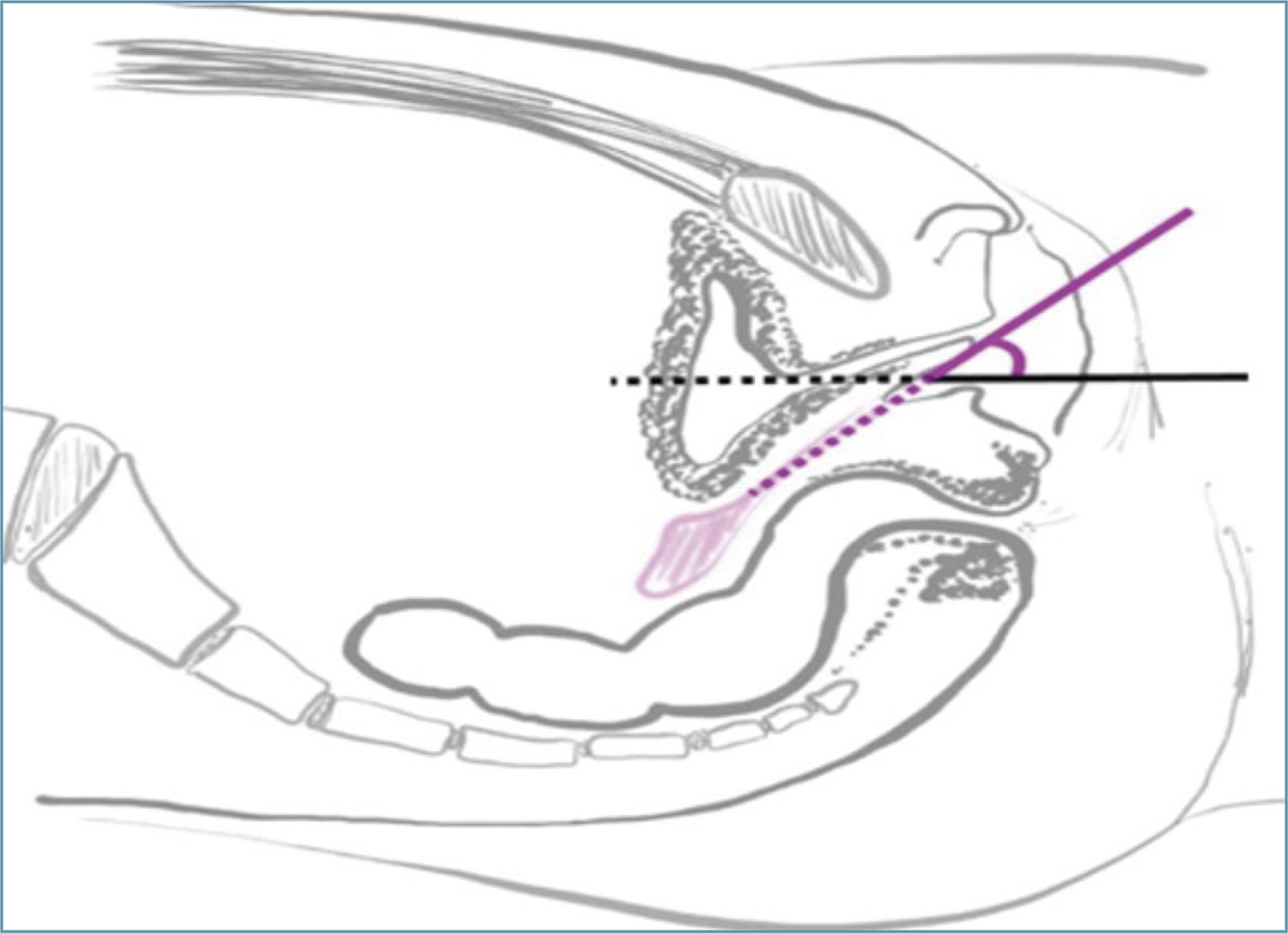
-
Original Article30/04/2025
Depression, anxiety, sexual function and quality of life in women with hyperprolactinemia
- Renan Massao Nakamura
 ,
, - Daniela Angerame Yela
 ,
, - Amanda Carvalho Santos
 ,
, - Beatriz Cipriano Ribas
 ,
, - Pedro Henrique Silva Rosa e
 , [ … ],
, [ … ], - Cristina Laguna Benetti-Pinto

Resumo
Original ArticleDepression, anxiety, sexual function and quality of life in women with hyperprolactinemia
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo7
- Renan Massao Nakamura
 ,
, - Daniela Angerame Yela
 ,
, - Amanda Carvalho Santos
 ,
, - Beatriz Cipriano Ribas
 ,
, - Pedro Henrique Silva Rosa e
 ,
, - Bianca Netto Motta
 ,
, - Gabriela Pravatta Rezende
 ,
, - Cristina Laguna Benetti-Pinto

Visualizações49Abstract
Objective:
To evaluate anxiety, depression, sexual function and quality of life in women with hyperprolactinemia.
Methods:
Cross-sectional study with 80 women divided into two groups: 30 women with hyperprolactinemia (Study Group) followed and treated at the endocrine gynecology outpatient clinic and 50 women without hyperprolactinemia, with regular menstrual cycles (Control Group) followed at the family planning outpatient clinic of the State University of Campinas from June 2021 to October 2022. Sociodemographic characteristics, quality of life (SF-36 Questionnaire), sexual function (Female Sexual Function Index Questionnaire), depression (Beck Depression Inventory) and anxiety (Beck Anxiety Scale) were evaluated in both groups. Categorical variables were described as absolute frequency and percentage; numerical variables as mean and standard deviation. Comparison of numerical variables between two groups was performed by Mann-Whitney test, while categorical were compared by Chi-Square or Fisher’s exact tests.
Results:
The mean age of women with hyperprolactinemia was 39.6±8.1 years and the Control Group was 31.2±9.5 years (p<0.001). There was no difference in anxiety scores (p=0.66), depression (p=0.08) and general sexual function (p=0.08) in both groups. However, women with hyperprolactinemia had lower scores in the domains of pain and arousal and worse functional capacity than Control Group (p<0.05).
Conclusion:
Women with hyperprolactinemia under treatment do not show any impairment in their anxiety, depression and sexual function when compared to women without hyperprolactinemia. However, analysis of quality of life showed that women with hyperprolactinemia have poor functional capacity.
Palavras-chave: AnxietyDepressionHyperpituitarismHyperprolactinemiaQuality of lifesexual functionsurveys and questionnairesVer maisVisualizações49

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleDepression, anxiety, sexual function and quality of life in women with hyperprolactinemia
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo7
- Renan Massao Nakamura
 ,
, - Daniela Angerame Yela
 ,
, - Amanda Carvalho Santos
 ,
, - Beatriz Cipriano Ribas
 ,
, - Pedro Henrique Silva Rosa e
 ,
, - Bianca Netto Motta
 ,
, - Gabriela Pravatta Rezende
 ,
, - Cristina Laguna Benetti-Pinto

Visualizações49Abstract
Objective:
To evaluate anxiety, depression, sexual function and quality of life in women with hyperprolactinemia.
Methods:
Cross-sectional study with 80 women divided into two groups: 30 women with hyperprolactinemia (Study Group) followed and treated at the endocrine gynecology outpatient clinic and 50 women without hyperprolactinemia, with regular menstrual cycles (Control Group) followed at the family planning outpatient clinic of the State University of Campinas from June 2021 to October 2022. Sociodemographic characteristics, quality of life (SF-36 Questionnaire), sexual function (Female Sexual Function Index Questionnaire), depression (Beck Depression Inventory) and anxiety (Beck Anxiety Scale) were evaluated in both groups. Categorical variables were described as absolute frequency and percentage; numerical variables as mean and standard deviation. Comparison of numerical variables between two groups was performed by Mann-Whitney test, while categorical were compared by Chi-Square or Fisher’s exact tests.
Results:
The mean age of women with hyperprolactinemia was 39.6±8.1 years and the Control Group was 31.2±9.5 years (p<0.001). There was no difference in anxiety scores (p=0.66), depression (p=0.08) and general sexual function (p=0.08) in both groups. However, women with hyperprolactinemia had lower scores in the domains of pain and arousal and worse functional capacity than Control Group (p<0.05).
Conclusion:
Women with hyperprolactinemia under treatment do not show any impairment in their anxiety, depression and sexual function when compared to women without hyperprolactinemia. However, analysis of quality of life showed that women with hyperprolactinemia have poor functional capacity.
Palavras-chave: AnxietyDepressionHyperpituitarismHyperprolactinemiaQuality of lifesexual functionsurveys and questionnairesVer mais

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. - Renan Massao Nakamura
-
Original Article30/04/2025
Hysterectomy rates per resident in final year of training in teaching hospitals: an ecologic study
- Luiza Nestori Chiozzotto
 ,
, - Nino José Wilson Moterani Júnior
 ,
, - Laura Bresciani Bento Gonçalves Moterani
 ,
, - Vinicius César Moterani
 ,
, - Francisco José Candido dos Reis

Resumo
Original ArticleHysterectomy rates per resident in final year of training in teaching hospitals: an ecologic study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo24
- Luiza Nestori Chiozzotto
 ,
, - Nino José Wilson Moterani Júnior
 ,
, - Laura Bresciani Bento Gonçalves Moterani
 ,
, - Vinicius César Moterani
 ,
, - Francisco José Candido dos Reis

Visualizações92Abstract
Objective:
Analyze the hysterectomy rates per resident in graduation year in teaching hospitals in the state of São Paulo (Brazil).
Methods:
We selected teaching hospitals in the state of São Paulo and gathered information from two public databases to estimate the hysterectomy rates per resident in their final year of training between 2009 and 2019.
Results:
Between 2009 and 2019, there was a 37.5% increase in the number of residents in their final year of training, a 4.31% increase in the number of hysterectomies, and a drop in the hysterectomy rates per resident of 24.1%. The reduction of the rate of hysterectomy per resident was more pronounced for vaginal route (46.4%) followed by abdominal route (23.3%). The ratio of laparoscopic hysterectomy per resident increased 264% during the period, however, this route was used in only 7% of the surgeries in 2019.
Conclusions:
The hysterectomy rates per resident in their final year of training showed a notable reduction. This trend, particularly pronounced in vaginal and abdominal routes, signals a shift towards minimally invasive techniques.
Palavras-chave: Clinical competenceEducation, medicalHospitals, teachingHysterectomylearning curveMedical staff, hospitalPhysiciansStudents, medicalSurgical procedures, operativeVer maisVisualizações92

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleHysterectomy rates per resident in final year of training in teaching hospitals: an ecologic study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo24
- Luiza Nestori Chiozzotto
 ,
, - Nino José Wilson Moterani Júnior
 ,
, - Laura Bresciani Bento Gonçalves Moterani
 ,
, - Vinicius César Moterani
 ,
, - Francisco José Candido dos Reis

Visualizações92Abstract
Objective:
Analyze the hysterectomy rates per resident in graduation year in teaching hospitals in the state of São Paulo (Brazil).
Methods:
We selected teaching hospitals in the state of São Paulo and gathered information from two public databases to estimate the hysterectomy rates per resident in their final year of training between 2009 and 2019.
Results:
Between 2009 and 2019, there was a 37.5% increase in the number of residents in their final year of training, a 4.31% increase in the number of hysterectomies, and a drop in the hysterectomy rates per resident of 24.1%. The reduction of the rate of hysterectomy per resident was more pronounced for vaginal route (46.4%) followed by abdominal route (23.3%). The ratio of laparoscopic hysterectomy per resident increased 264% during the period, however, this route was used in only 7% of the surgeries in 2019.
Conclusions:
The hysterectomy rates per resident in their final year of training showed a notable reduction. This trend, particularly pronounced in vaginal and abdominal routes, signals a shift towards minimally invasive techniques.
Palavras-chave: Clinical competenceEducation, medicalHospitals, teachingHysterectomylearning curveMedical staff, hospitalPhysiciansStudents, medicalSurgical procedures, operativeVer mais

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. 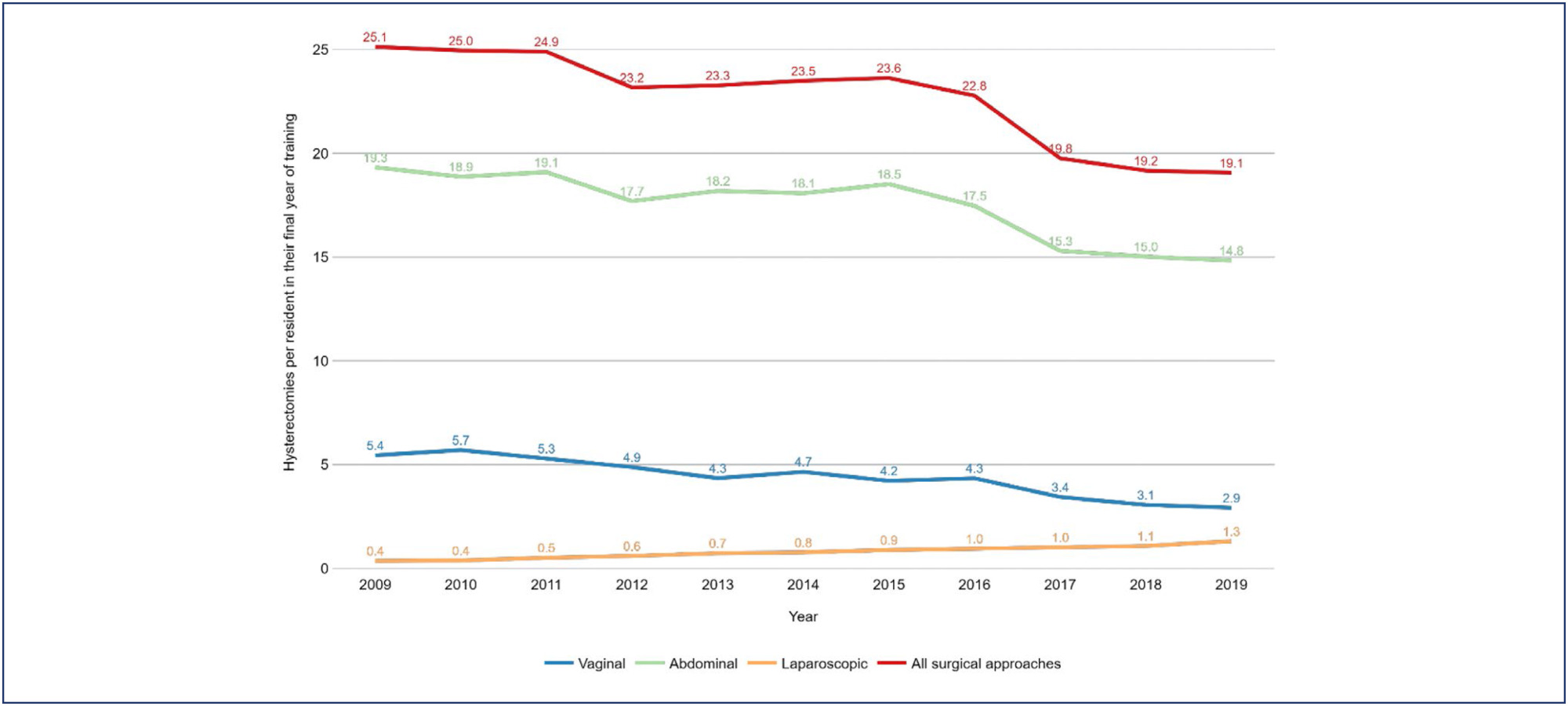
- Luiza Nestori Chiozzotto
-
Original Article30/04/2025
Prevalence of antiphospholipid syndrome among women with recurrent pregnancy loss: a cohort study
- Elaine Cristina Fontes de Oliveira
 ,
, - Daniel Dias Ribeiro
 ,
, - Janaína Campos Senra
 ,
, - Fernando Marcos dos Reis

Resumo
Original ArticlePrevalence of antiphospholipid syndrome among women with recurrent pregnancy loss: a cohort study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo23
- Elaine Cristina Fontes de Oliveira
 ,
, - Daniel Dias Ribeiro
 ,
, - Janaína Campos Senra
 ,
, - Fernando Marcos dos Reis

Visualizações83Abstract
Objective:
This study aimed to evaluate the prevalence of antiphospholipid syndrome (APS) among women experiencing recurrent pregnancy loss (RPL).
Methods:
A cross-sectional was conducted, reviewing the medical records of 134 women with a history of two or more miscarriages, treated between January 2014 and May 2024 at a tertiary university center in Belo Horizonte, Brazil. APS screening was performed by assessing anticardiolipin (IgG and IgM), lupus anticoagulant, and anti-β2-glycoprotein-1 (IgG and IgM) antibodies, based on Sapporo criteria. All tests were performed during non-pregnant periods and at least 12 weeks after the last miscarriage.
Results:
The study included 134 women with a mean age of 33.8 ± 5.7 years. The number of prior miscarriages ranged from 2 to 11 per couple. Among the patients who presented the lupus anticoagulant, only two (1.49%) tested positive in two samples, as per revised Sapporo criteria. Considering IgG and IgM anticardiolipin antibodies, four patients (2.98%) tested positive in two samples according to old Sapporo criteria, with one patient having a positive IgG test in two samples, two having positive IgM in two samples and a single patient having both positive tests. None of the 56 patients tested positive for anti-β2-glycoprotein-1 antibodies in two samples.
Conclusion:
The prevalence of antiphospholipid antibodies, in line with revised Sapporo criteria, is low among Brazilian women with recurrent pregnancy loss, consistent with recent studies in literature. Ensuring the appropriateness of diagnostic criteria is crucial to avoid unnecessary treatment with platelet anticoagulants and heparin in this population.
Palavras-chave: Abortion, habitualAbortion, spontaneousAntibodiesAnticardiolipinAntiphospholipid syndromePrevalenceThrombophiliaVer maisVisualizações83

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticlePrevalence of antiphospholipid syndrome among women with recurrent pregnancy loss: a cohort study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo23
- Elaine Cristina Fontes de Oliveira
 ,
, - Daniel Dias Ribeiro
 ,
, - Janaína Campos Senra
 ,
, - Fernando Marcos dos Reis

Visualizações83Abstract
Objective:
This study aimed to evaluate the prevalence of antiphospholipid syndrome (APS) among women experiencing recurrent pregnancy loss (RPL).
Methods:
A cross-sectional was conducted, reviewing the medical records of 134 women with a history of two or more miscarriages, treated between January 2014 and May 2024 at a tertiary university center in Belo Horizonte, Brazil. APS screening was performed by assessing anticardiolipin (IgG and IgM), lupus anticoagulant, and anti-β2-glycoprotein-1 (IgG and IgM) antibodies, based on Sapporo criteria. All tests were performed during non-pregnant periods and at least 12 weeks after the last miscarriage.
Results:
The study included 134 women with a mean age of 33.8 ± 5.7 years. The number of prior miscarriages ranged from 2 to 11 per couple. Among the patients who presented the lupus anticoagulant, only two (1.49%) tested positive in two samples, as per revised Sapporo criteria. Considering IgG and IgM anticardiolipin antibodies, four patients (2.98%) tested positive in two samples according to old Sapporo criteria, with one patient having a positive IgG test in two samples, two having positive IgM in two samples and a single patient having both positive tests. None of the 56 patients tested positive for anti-β2-glycoprotein-1 antibodies in two samples.
Conclusion:
The prevalence of antiphospholipid antibodies, in line with revised Sapporo criteria, is low among Brazilian women with recurrent pregnancy loss, consistent with recent studies in literature. Ensuring the appropriateness of diagnostic criteria is crucial to avoid unnecessary treatment with platelet anticoagulants and heparin in this population.
Palavras-chave: Abortion, habitualAbortion, spontaneousAntibodiesAnticardiolipinAntiphospholipid syndromePrevalenceThrombophiliaVer mais

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. - Elaine Cristina Fontes de Oliveira
-
Original Article30/04/2025
An assessment of total antioxidant and oxidant parameters and their correlation with embryo quality in in-vitro fertilization patients
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo22
Resumo
Original ArticleAn assessment of total antioxidant and oxidant parameters and their correlation with embryo quality in in-vitro fertilization patients
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo22
Visualizações80Abstract
Objective:
In vitro, fertilization is the primary treatment method for infertility. Follicular fluid analysis is an approach used to optimize the results of assisted reproductive techniques. Oxidative stress represents the imbalance between the production of reactive oxygen species and their detoxification. Total Antioxidant and Oxidant Status, and Oxidative Stress Index levels are the main oxidative stress markers. This study investigated the effects of oxidative stress markers on infertility etiology, embryo quality, and success of In vitro fertilization.
Methods:
Before enrolling in the ICSI-ET cycle, participants had their FSH and LH levels assessed on the second day of the cycle. The ovarian degrees of the participants were evaluated by transvaginal ultrasonography. Participants underwent controlled ovarian stimulation using the GnRH antagonist protocol. TV-USG and serial E2 measurements were performed at appropriate intervals to follow follicular development. Follicle sizes, quantity, and endometrial thickness were recorded. Total Antioxidant and Oxidant Status, and Oxidative analyses were conducted using Rel Assay Diagnostics Assay Kits.
Results:
The average number of total oocytes in the participants was 10.25±6.66, and the average of mature M2 stage oocytes was 6.71±3.72. The average number of fertilized oocytes was 4.65±2.81. Fertilization rates were calculated as approximately 54.75±25.58%. A statistically significant positive correlation was found between embryo quality and serum Total Antioxidant Status levels (p=0.004). Similarly, a significant positive correlation was observed between embryo quality and follicular Total Antioxidant Status values (r = 0.42, p = 0.01).
Conclusion:
This study concluded that oxidative stress markers affect certain stages of the IVF treatment process.
Palavras-chave: AntioxidantsFertilization in vitroFollicular fluidInfertilityOocytesOxidantsOxidative stressVer maisVisualizações80

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleAn assessment of total antioxidant and oxidant parameters and their correlation with embryo quality in in-vitro fertilization patients
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo22
Visualizações80Abstract
Objective:
In vitro, fertilization is the primary treatment method for infertility. Follicular fluid analysis is an approach used to optimize the results of assisted reproductive techniques. Oxidative stress represents the imbalance between the production of reactive oxygen species and their detoxification. Total Antioxidant and Oxidant Status, and Oxidative Stress Index levels are the main oxidative stress markers. This study investigated the effects of oxidative stress markers on infertility etiology, embryo quality, and success of In vitro fertilization.
Methods:
Before enrolling in the ICSI-ET cycle, participants had their FSH and LH levels assessed on the second day of the cycle. The ovarian degrees of the participants were evaluated by transvaginal ultrasonography. Participants underwent controlled ovarian stimulation using the GnRH antagonist protocol. TV-USG and serial E2 measurements were performed at appropriate intervals to follow follicular development. Follicle sizes, quantity, and endometrial thickness were recorded. Total Antioxidant and Oxidant Status, and Oxidative analyses were conducted using Rel Assay Diagnostics Assay Kits.
Results:
The average number of total oocytes in the participants was 10.25±6.66, and the average of mature M2 stage oocytes was 6.71±3.72. The average number of fertilized oocytes was 4.65±2.81. Fertilization rates were calculated as approximately 54.75±25.58%. A statistically significant positive correlation was found between embryo quality and serum Total Antioxidant Status levels (p=0.004). Similarly, a significant positive correlation was observed between embryo quality and follicular Total Antioxidant Status values (r = 0.42, p = 0.01).
Conclusion:
This study concluded that oxidative stress markers affect certain stages of the IVF treatment process.
Palavras-chave: AntioxidantsFertilization in vitroFollicular fluidInfertilityOocytesOxidantsOxidative stressVer mais

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. 
-
Review Article30/04/2025
Letrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
- Karine Eskandar
 ,
, - Juliana Almeida Oliveira
 ,
, - Sandro Augusto Ribeiro
 ,
, - Matheus Pedrotti Chavez
 ,
, - Ana Isabela de Araujo Zotti
 , [ … ],
, [ … ], - Andrea Mora de Marco Novellino

Resumo
Review ArticleLetrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
- Karine Eskandar
 ,
, - Juliana Almeida Oliveira
 ,
, - Sandro Augusto Ribeiro
 ,
, - Matheus Pedrotti Chavez
 ,
, - Ana Isabela de Araujo Zotti
 ,
, - Yasmin Jardim Meirelles Dias
 ,
, - Andrea Mora de Marco Novellino

Visualizações93Abstract
Objective:
We aimed to compare the efficacy and safety of letrozole and clomiphene versus letrozole alone for ovulation induction in patients with Polycystic Ovary Syndrome (PCOS).
Data Sources:
We systematically searched EMBASE, PubMed, and Cochrane databases on October 31, 2024.
Study selection:
We included studies of women with PCOS treated with a combination of clomiphene and letrozole or letrozole alone to induce ovulation that reported any of the outcomes of interest, namely rate of mature follicles and ovulation, ovulation, pregnancy, miscarriages, endometrial thickness, and number of mature follicles.
Data collection:
We pooled odds ratios (OR) and mean difference (MD) with 95% confidence intervals (CI) using a random effects model using R statistical software, version 4.2.1. Heterogeneity was assessed with I statistics, and a random effects model was used.
Data Synthesis:
Four RCTs and two observational studies comprising 592 patients were included. Combined therapy was associated with a higher rate of a mature follicle (OR 2.74; 95% CI 1.72-4.37; p< 0.001; I=0%) and ovulation (OR 2.55; 95% CI 1.57-4.12; p< 0.001; I=35.9%). The number of mature follicles, number of pregnancies, thickness of endometrial lining, and the incidence of adverse events, including headache, abdominal bloating, fatigue, back pain, breast discomfort, and night sweats, were similar between groups.
Conclusion:
In women with anovulatory infertility secondary to PCOS, letrozole and clomiphene citrate combined therapy was associated with improved mature follicle and ovulation rates, with a similar safety profile compared to letrozole alone. However, no significant impact was observed on pregnancy rates.
Palavras-chave: ClomipheneInfertility, femaleLetrozoleOvulationOvulation InductionPolycystic ovary syndromeVer maisVisualizações93

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Review ArticleLetrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
- Karine Eskandar
 ,
, - Juliana Almeida Oliveira
 ,
, - Sandro Augusto Ribeiro
 ,
, - Matheus Pedrotti Chavez
 ,
, - Ana Isabela de Araujo Zotti
 ,
, - Yasmin Jardim Meirelles Dias
 ,
, - Andrea Mora de Marco Novellino

Visualizações93Abstract
Objective:
We aimed to compare the efficacy and safety of letrozole and clomiphene versus letrozole alone for ovulation induction in patients with Polycystic Ovary Syndrome (PCOS).
Data Sources:
We systematically searched EMBASE, PubMed, and Cochrane databases on October 31, 2024.
Study selection:
We included studies of women with PCOS treated with a combination of clomiphene and letrozole or letrozole alone to induce ovulation that reported any of the outcomes of interest, namely rate of mature follicles and ovulation, ovulation, pregnancy, miscarriages, endometrial thickness, and number of mature follicles.
Data collection:
We pooled odds ratios (OR) and mean difference (MD) with 95% confidence intervals (CI) using a random effects model using R statistical software, version 4.2.1. Heterogeneity was assessed with I statistics, and a random effects model was used.
Data Synthesis:
Four RCTs and two observational studies comprising 592 patients were included. Combined therapy was associated with a higher rate of a mature follicle (OR 2.74; 95% CI 1.72-4.37; p< 0.001; I=0%) and ovulation (OR 2.55; 95% CI 1.57-4.12; p< 0.001; I=35.9%). The number of mature follicles, number of pregnancies, thickness of endometrial lining, and the incidence of adverse events, including headache, abdominal bloating, fatigue, back pain, breast discomfort, and night sweats, were similar between groups.
Conclusion:
In women with anovulatory infertility secondary to PCOS, letrozole and clomiphene citrate combined therapy was associated with improved mature follicle and ovulation rates, with a similar safety profile compared to letrozole alone. However, no significant impact was observed on pregnancy rates.
Palavras-chave: ClomipheneInfertility, femaleLetrozoleOvulationOvulation InductionPolycystic ovary syndromeVer mais

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. 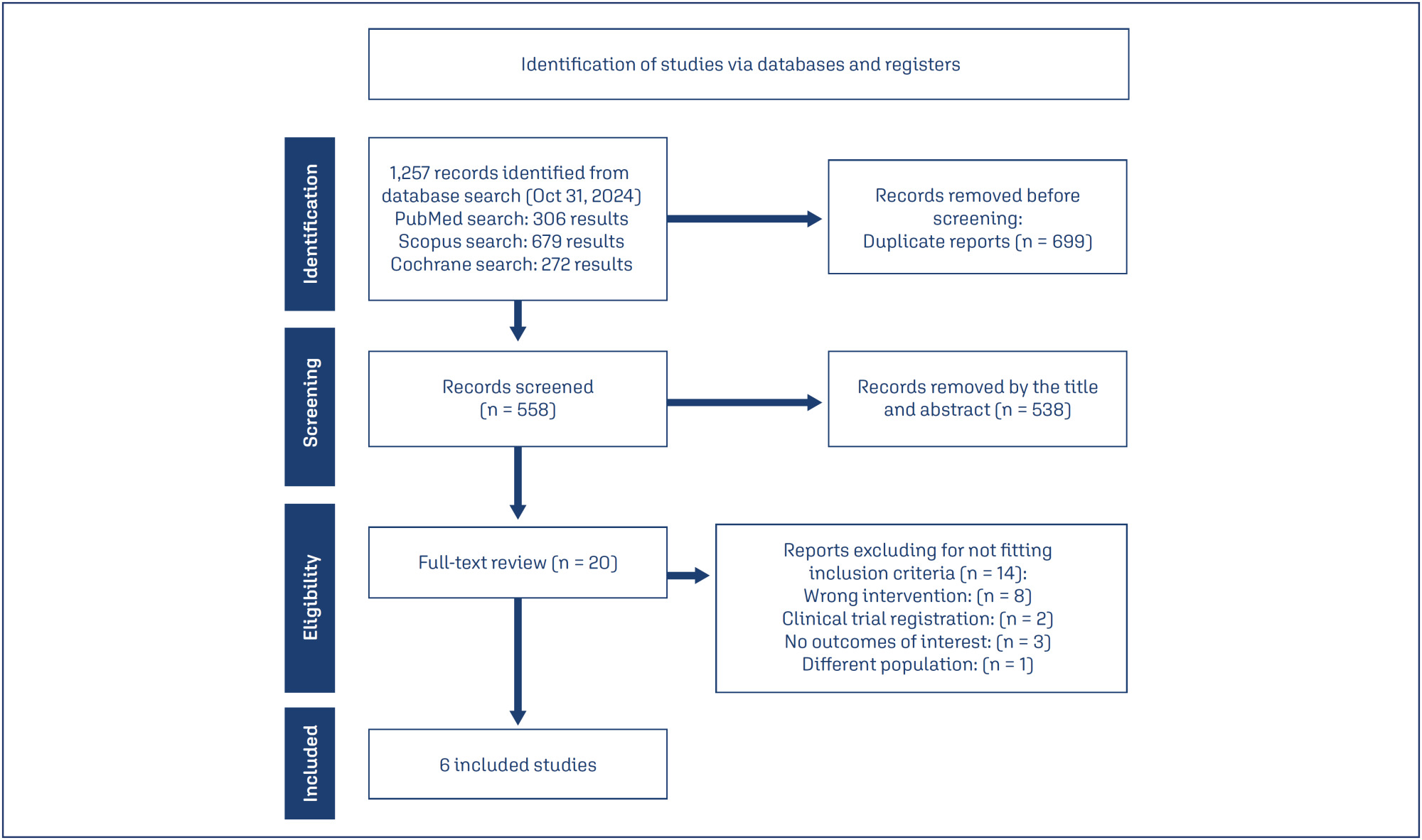
- Karine Eskandar
-
Original Article30/04/2025
Incidence of small-for-gestational-age newborns in pregnant women with COVID-19
- Gustavo dos Santos Raupp
 ,
, - Renato Teixeira Souza
 ,
, - Maria Laura Costa
 ,
, - Jose Guilherme Cecatti
 ,
, - Annerose Barros
 , [ … ],
, [ … ], - Janete Vettorazzi

Resumo
Original ArticleIncidence of small-for-gestational-age newborns in pregnant women with COVID-19
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo20
- Gustavo dos Santos Raupp
 ,
, - Renato Teixeira Souza
 ,
, - Maria Laura Costa
 ,
, - Jose Guilherme Cecatti
 ,
, - Annerose Barros
 ,
, - Ellen Machado Arlindo
 ,
, - Edson Vieira Cunha Filho
 ,
, - Janete Vettorazzi

Visualizações77Abstract
Objective:
This study aimed to assess the incidence of small for gestational age (SGA) newborns in pregnant women infected with COVID-19 and examine the associated neonatal outcomes.
Methods:
This study involved a secondary analysis of the REBRACO Network, a prospective cohort study conducted in 15 maternity hospitals in Brazil before the introduction of COVID-19 vaccination (February 2020 to February 2021). Demographic data of pregnant women tested for COVID-19 were analyzed, and fetal outcomes were compared between women with positive and negative COVID-19 results who had SGA fetuses.
Results:
A total of 729 symptomatic pregnant women with COVID-19 were included in the study. However, there were 248 participants with missing information regarding childbirth or loss of follow-up, and 107 participants without confirmatory tests for COVID-19. Among the remaining participants, 198 had confirmed COVID-19 and 176 tested negative. The incidence of SGA among women with COVID-19 was 22.4%, whereas the incidence among women who tested negative for COVID-19 was 14.8%. SGA newborns born to COVID-19 positive pregnant women were 1.6 times more likely to experience adverse outcomes (such as prematurity, stillbirth, neonatal death, and admission to a neonatal ICU) compared to non-SGA newborns [OR = 1.655 (1.145 – 2.394); P=0.017]. In SGA newborns of pregnant women with confirmed COVID-19 infection, mechanical ventilation use was found to be associated with the infection [OR = 0.692 (0.562 – 0.853); P=0.002].
Conclusion:
The higher incidence of SGA newborns and its stronger association with prematurity in pregnant women with confirmed COVID-19 infection suggest that COVID-19 infection is a significant factor contributing to neonatal morbidity and mortality.
Palavras-chave: coronavirus infectionsCOVID-19Infant, newbornInfant, small for gestational agematernal healthPregnancy complicationsVer maisVisualizações77

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleIncidence of small-for-gestational-age newborns in pregnant women with COVID-19
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo20
- Gustavo dos Santos Raupp
 ,
, - Renato Teixeira Souza
 ,
, - Maria Laura Costa
 ,
, - Jose Guilherme Cecatti
 ,
, - Annerose Barros
 ,
, - Ellen Machado Arlindo
 ,
, - Edson Vieira Cunha Filho
 ,
, - Janete Vettorazzi

Visualizações77Abstract
Objective:
This study aimed to assess the incidence of small for gestational age (SGA) newborns in pregnant women infected with COVID-19 and examine the associated neonatal outcomes.
Methods:
This study involved a secondary analysis of the REBRACO Network, a prospective cohort study conducted in 15 maternity hospitals in Brazil before the introduction of COVID-19 vaccination (February 2020 to February 2021). Demographic data of pregnant women tested for COVID-19 were analyzed, and fetal outcomes were compared between women with positive and negative COVID-19 results who had SGA fetuses.
Results:
A total of 729 symptomatic pregnant women with COVID-19 were included in the study. However, there were 248 participants with missing information regarding childbirth or loss of follow-up, and 107 participants without confirmatory tests for COVID-19. Among the remaining participants, 198 had confirmed COVID-19 and 176 tested negative. The incidence of SGA among women with COVID-19 was 22.4%, whereas the incidence among women who tested negative for COVID-19 was 14.8%. SGA newborns born to COVID-19 positive pregnant women were 1.6 times more likely to experience adverse outcomes (such as prematurity, stillbirth, neonatal death, and admission to a neonatal ICU) compared to non-SGA newborns [OR = 1.655 (1.145 – 2.394); P=0.017]. In SGA newborns of pregnant women with confirmed COVID-19 infection, mechanical ventilation use was found to be associated with the infection [OR = 0.692 (0.562 – 0.853); P=0.002].
Conclusion:
The higher incidence of SGA newborns and its stronger association with prematurity in pregnant women with confirmed COVID-19 infection suggest that COVID-19 infection is a significant factor contributing to neonatal morbidity and mortality.
Palavras-chave: coronavirus infectionsCOVID-19Infant, newbornInfant, small for gestational agematernal healthPregnancy complicationsVer mais

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. 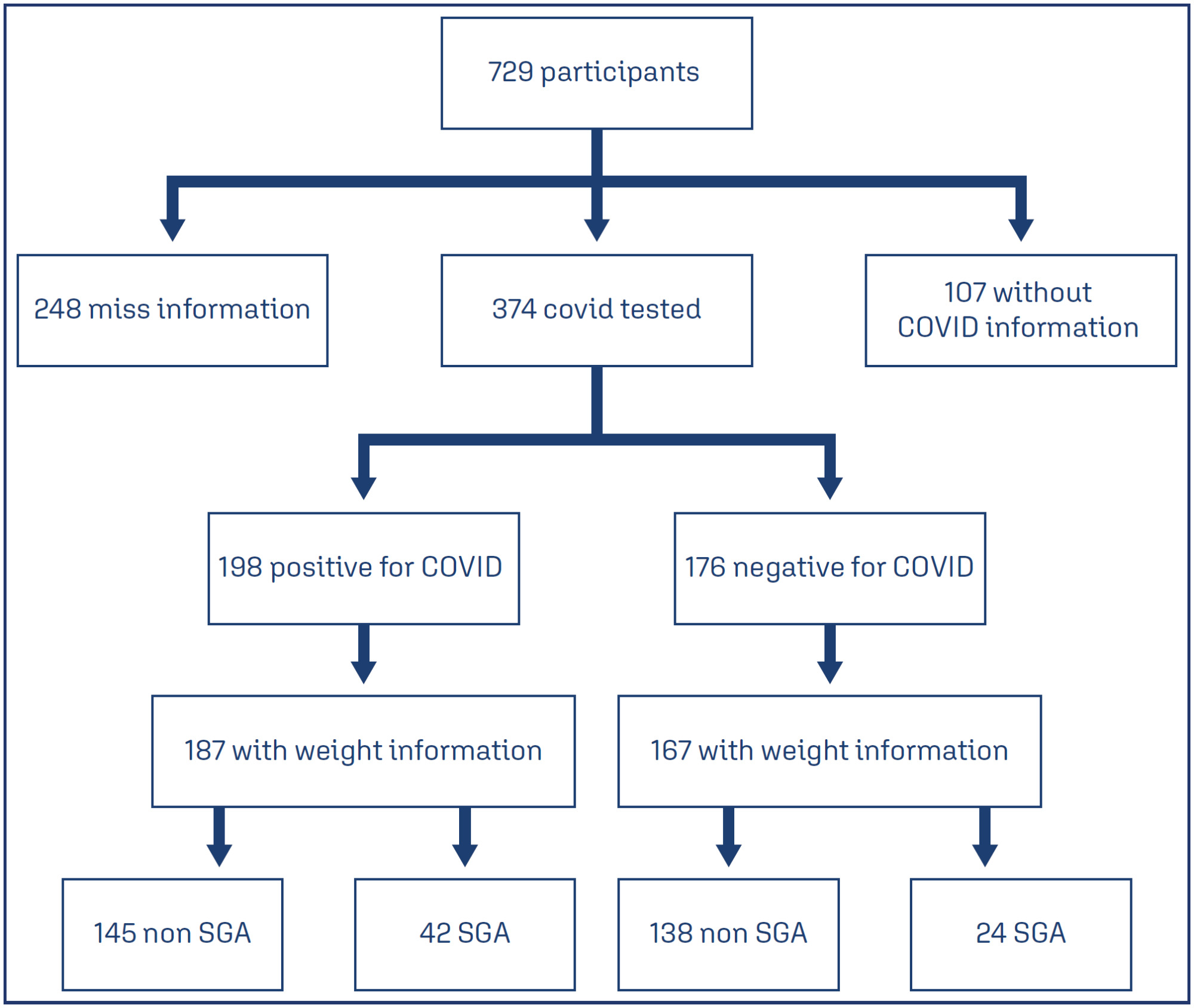
- Gustavo dos Santos Raupp
-
Review Article30/04/2025
Efficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
- Nicole Cristina Lottermann
 ,
, - Nathalia Luiza Andreazza
 ,
, - Matheus de Araújo Moura Cavalcante
 ,
, - Laura Andrade Fernandez
 ,
, - Carla Vitola Gonçalvez
 , [ … ],
, [ … ], - Linjie Zhang

Resumo
Review ArticleEfficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo18
- Nicole Cristina Lottermann
 ,
, - Nathalia Luiza Andreazza
 ,
, - Matheus de Araújo Moura Cavalcante
 ,
, - Laura Andrade Fernandez
 ,
, - Carla Vitola Gonçalvez
 ,
, - Linjie Zhang

Visualizações82Abstract
Objective:
This umbrella review aimed to synthesize evidence from systematic reviews of clinical trials on the efficacy of tranexamic acid in gynecology and obstetrics procedures.
Methods:
We searched Medline, Embase, SciELO and Cochrane Database of Systematic Reviews on March 11, 2024, using the term “tranexamic acid”. Four reviewers independently select studies and extract data. We assessed the quality of systematic review and the quality of evidence, using AMSTAR 2 and GRADE tools, respectively.
Results:
Of 651 systematic reviews identified, 16 reviews with 96663 patients were included. The surgical procedures were cesarean section, myomectomy, hysterectomy, and cervical intraepithelial neoplasia surgery. All reviews showed a statistically significant and clinically relevant reduction in intraoperative and post-procedure blood loss, associated with intravenous or topical use of tranexamic acid. Tranexamic acid resulted in a significant reduction in the need for blood transfusions and a less pronounced drop in postoperative hematocrit and hemoglobin levels in cesarean section. Several reviews addressed the same question, but the number of included trials varied substantially, which might indicate flaws in search and selection of studies of these reviews. The quality of systematic reviews was low or critically low, and the quality of evidence was moderate.
Conclusions:
This umbrella review shows that tranexamic acid can reduce blood loss and hemorrhage in gynecology and obstetrics procedures. High quality systematic reviews are still needed.
Palavras-chave: Blood transfusionCesarean sectionEfficacyGynecologic surgical procedureshematocritHemorrhageHysterectomyObstetric surgical proceduresTranexamic acidUterine cervical dysplasiauterine myomectomyVer maisVisualizações82

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Review ArticleEfficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo18
- Nicole Cristina Lottermann
 ,
, - Nathalia Luiza Andreazza
 ,
, - Matheus de Araújo Moura Cavalcante
 ,
, - Laura Andrade Fernandez
 ,
, - Carla Vitola Gonçalvez
 ,
, - Linjie Zhang

Visualizações82Abstract
Objective:
This umbrella review aimed to synthesize evidence from systematic reviews of clinical trials on the efficacy of tranexamic acid in gynecology and obstetrics procedures.
Methods:
We searched Medline, Embase, SciELO and Cochrane Database of Systematic Reviews on March 11, 2024, using the term “tranexamic acid”. Four reviewers independently select studies and extract data. We assessed the quality of systematic review and the quality of evidence, using AMSTAR 2 and GRADE tools, respectively.
Results:
Of 651 systematic reviews identified, 16 reviews with 96663 patients were included. The surgical procedures were cesarean section, myomectomy, hysterectomy, and cervical intraepithelial neoplasia surgery. All reviews showed a statistically significant and clinically relevant reduction in intraoperative and post-procedure blood loss, associated with intravenous or topical use of tranexamic acid. Tranexamic acid resulted in a significant reduction in the need for blood transfusions and a less pronounced drop in postoperative hematocrit and hemoglobin levels in cesarean section. Several reviews addressed the same question, but the number of included trials varied substantially, which might indicate flaws in search and selection of studies of these reviews. The quality of systematic reviews was low or critically low, and the quality of evidence was moderate.
Conclusions:
This umbrella review shows that tranexamic acid can reduce blood loss and hemorrhage in gynecology and obstetrics procedures. High quality systematic reviews are still needed.
Palavras-chave: Blood transfusionCesarean sectionEfficacyGynecologic surgical procedureshematocritHemorrhageHysterectomyObstetric surgical proceduresTranexamic acidUterine cervical dysplasiauterine myomectomyVer mais

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. 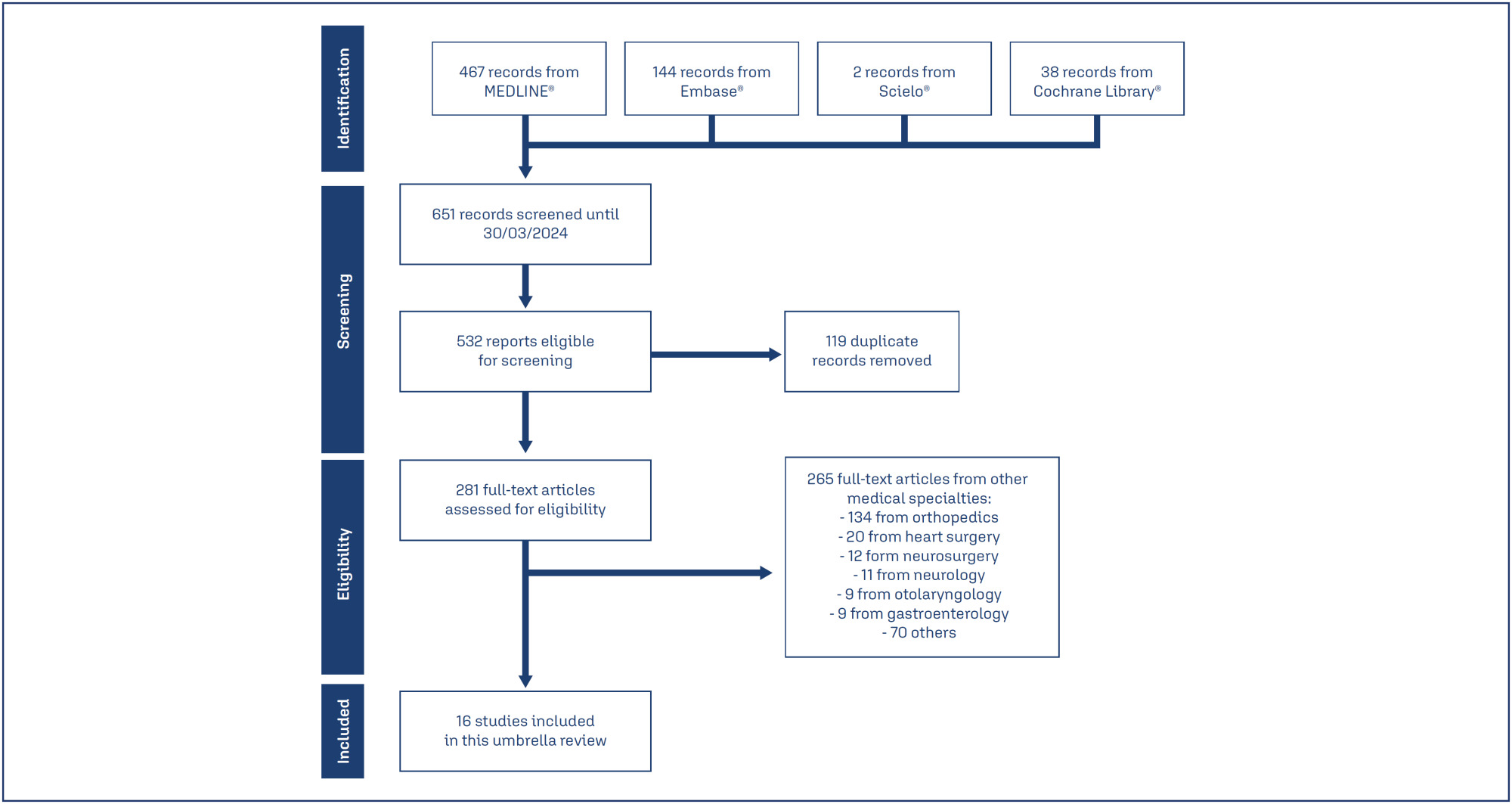
- Nicole Cristina Lottermann
Busca
Pesquisar em:
Nuvem de Tags
Gravidez (167)Fatores de risco (89)Menopausa (79)Pré-eclâmpsia (66)Endometriose (65)Mama (59)Infertilidade (58)Obesidade (57)Complicações na gravidez (56)Diagnóstico pré-natal (54)Gestação (54)Qualidade de vida (53)Saúde da mulher (51)Cesárea (50)Complicações da gravidez (50)Neoplasias da mama (49)Fertilização in vitro (48)Cuidado pré-natal (47)Mortalidade materna (43)Ultra-sonografia (43)
Artigos em destaque
- FEBRASGO POSITION STATEMENT18/03/2025
Use of synthetic slings in the treatment of female stress urinary incontinence: Number 2 – 2025
- Marair Gracio Ferreira Sartori
 ,
, - Marilene Vale de Castro Monteiro
 ,
, - Cássia Raquel Teatin Juliato
 ,
, - Luiz Gustavo Oliveira Brito
 ,
, - Sergio Brasileiro Martins
 ,
, - José Miguel de Deus
 ,
, - Ana Selma Bertelli Picoloto
 ,
, - Jorge Milhem Haddad
 ,
, - Andreisa Paiva Monteiro Bilhar
 ,
, - Leticia Maria de Oliveira
 ,
, - Rafael Mendes Moroni
 ,
, - Lucas Schreiner
 ,
, - Aljerry Dias do Rego
 ,
, - Daniela Siqueira Prado
 ,
, - Emerson de Oliveira

Resumo
FEBRASGO POSITION STATEMENTUse of synthetic slings in the treatment of female stress urinary incontinence: Number 2 – 2025
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-FPS2
- Marair Gracio Ferreira Sartori
 ,
, - Marilene Vale de Castro Monteiro
 ,
, - Cássia Raquel Teatin Juliato
 ,
, - Luiz Gustavo Oliveira Brito
 ,
, - Sergio Brasileiro Martins
 ,
, - José Miguel de Deus
 ,
, - Ana Selma Bertelli Picoloto
 ,
, - Jorge Milhem Haddad
 ,
, - Andreisa Paiva Monteiro Bilhar
 ,
, - Leticia Maria de Oliveira
 ,
, - Rafael Mendes Moroni
 ,
, - Lucas Schreiner
 ,
, - Aljerry Dias do Rego
 ,
, - Daniela Siqueira Prado
 ,
, - Emerson de Oliveira

Visualizações174

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
FEBRASGO POSITION STATEMENTUse of synthetic slings in the treatment of female stress urinary incontinence: Number 2 – 2025
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-FPS2
- Marair Gracio Ferreira Sartori
 ,
, - Marilene Vale de Castro Monteiro
 ,
, - Cássia Raquel Teatin Juliato
 ,
, - Luiz Gustavo Oliveira Brito
 ,
, - Sergio Brasileiro Martins
 ,
, - José Miguel de Deus
 ,
, - Ana Selma Bertelli Picoloto
 ,
, - Jorge Milhem Haddad
 ,
, - Andreisa Paiva Monteiro Bilhar
 ,
, - Leticia Maria de Oliveira
 ,
, - Rafael Mendes Moroni
 ,
, - Lucas Schreiner
 ,
, - Aljerry Dias do Rego
 ,
, - Daniela Siqueira Prado
 ,
, - Emerson de Oliveira



This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. - Marair Gracio Ferreira Sartori
- Original Article18/03/2025
The experience of pregnancy in the COVID-19 pandemic
- Mariana Corniani Lopes
 ,
, - Cheryl Tatano Beck
 ,
, - Zelina Hilária de Souza Rosa
 ,
, - Erika de Sá Vieira Abuchaim

Resumo
Original ArticleThe experience of pregnancy in the COVID-19 pandemic
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo8
- Mariana Corniani Lopes
 ,
, - Cheryl Tatano Beck
 ,
, - Zelina Hilária de Souza Rosa
 ,
, - Erika de Sá Vieira Abuchaim

Visualizações182Ver maisAbstract
Objective:
To describe women’s experience of pregnancy during the COVID-19 pandemic.
Methods:
A qualitative study conducted in a private maternity hospital, from May, 2020 to November, 2021, with women aged ≥ 18 years, gestational age ≥ 36 weeks at birth and ≥ 24 hours post-partum. Data collected through semi-structured interviews, recorded, transcribed, and analyzed adopting Krippendorff’s Content Analysis as theoretical-methodological framework.
Results:
Four main themes emerged: Fear, Taking care and celebrating pregnancy: adjusting to the new reality, Harms of Isolation, and Benefits of Isolation. The fear of contamination and its impact on the health of mother and child resulted in the adoption of severe social isolation, including from those considered sources of support by the expecting mother. Overwhelmed, some of the participants reported loneliness and psychic suffering. The opportunity to focus on the pregnancy, the preparations for the arrival of the child, and the family made isolation a beneficial and positive period for other women.
Conclusion:
The experience of pregnancy in the Pandemic was an event outside of the ordinary and common. The expecting mother faced her worst fears on a daily basis and attended prenatal care, in order to ensure her child would be born healthy. The celebration of the baby’s life, amid so many deaths, had to be adjusted to the virtual environment. It was a tense, solitary, and ambiguous period, which demanded a lot from the mental health of some participants, but to others, brought advantages that would not have been possible in different times.
Visualizações182

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleThe experience of pregnancy in the COVID-19 pandemic
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo8
- Mariana Corniani Lopes
 ,
, - Cheryl Tatano Beck
 ,
, - Zelina Hilária de Souza Rosa
 ,
, - Erika de Sá Vieira Abuchaim

Visualizações182Ver maisAbstract
Objective:
To describe women’s experience of pregnancy during the COVID-19 pandemic.
Methods:
A qualitative study conducted in a private maternity hospital, from May, 2020 to November, 2021, with women aged ≥ 18 years, gestational age ≥ 36 weeks at birth and ≥ 24 hours post-partum. Data collected through semi-structured interviews, recorded, transcribed, and analyzed adopting Krippendorff’s Content Analysis as theoretical-methodological framework.
Results:
Four main themes emerged: Fear, Taking care and celebrating pregnancy: adjusting to the new reality, Harms of Isolation, and Benefits of Isolation. The fear of contamination and its impact on the health of mother and child resulted in the adoption of severe social isolation, including from those considered sources of support by the expecting mother. Overwhelmed, some of the participants reported loneliness and psychic suffering. The opportunity to focus on the pregnancy, the preparations for the arrival of the child, and the family made isolation a beneficial and positive period for other women.
Conclusion:
The experience of pregnancy in the Pandemic was an event outside of the ordinary and common. The expecting mother faced her worst fears on a daily basis and attended prenatal care, in order to ensure her child would be born healthy. The celebration of the baby’s life, amid so many deaths, had to be adjusted to the virtual environment. It was a tense, solitary, and ambiguous period, which demanded a lot from the mental health of some participants, but to others, brought advantages that would not have been possible in different times.


This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. 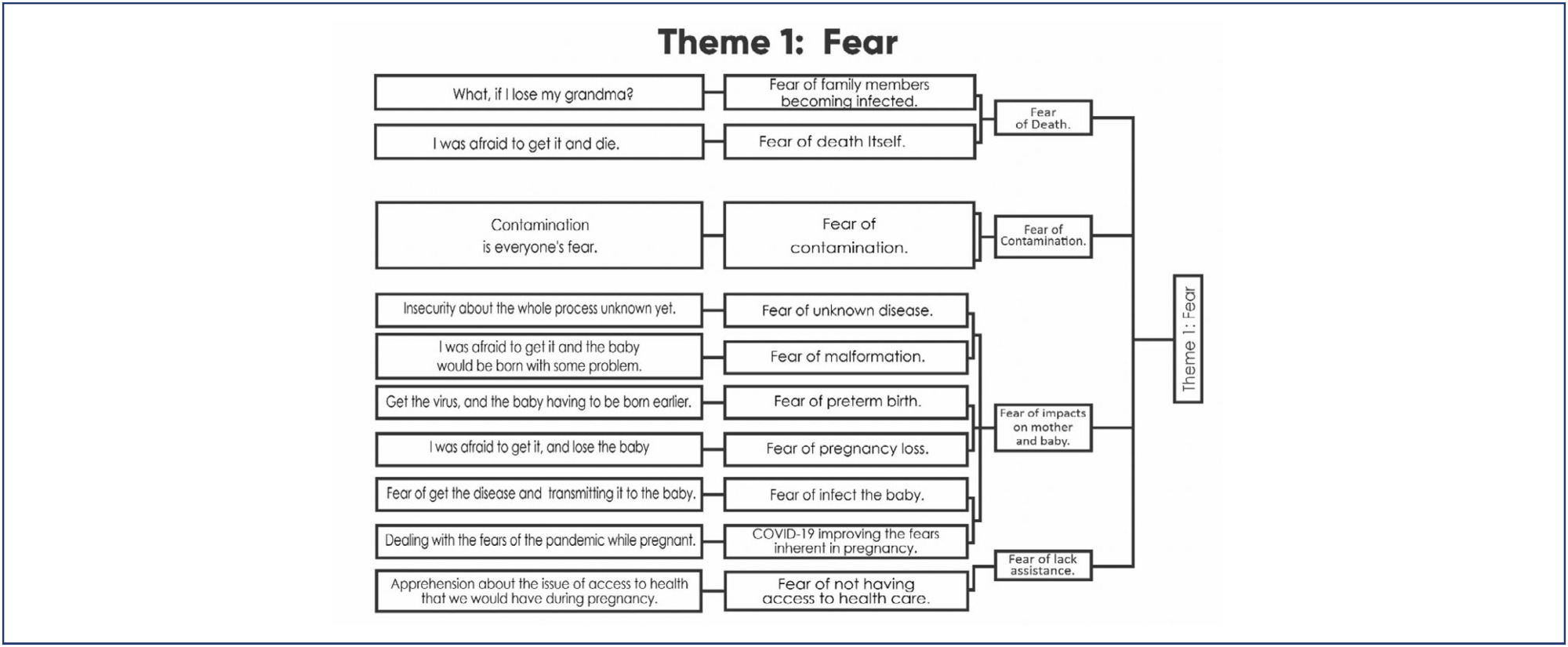
- Mariana Corniani Lopes
- Original Article13/02/2025
Anemia levels in the preconception period and the first trimester of pregnancy: a national, multicentric and cross-sectional study
- Aytaj Jafarzade
 ,
, - Veli Mi̇hmanli
 ,
, - And Yavuz
 ,
, - Murat Akbaş
 ,
, - Gürcan Türkyilmaz
 ,
, - Esra Nur Özkan
 ,
, - Murat İbrahim Toplu
 ,
, - Yücel Kaya
 ,
, - Damla Yasemin Yenli̇k Kaya
 ,
, - Mustafa Yildiz
 ,
, - Ali Emre Ati̇k
 ,
, - Elif İlgazi̇ Kiliç
 ,
, - Burcu Özata
 ,
, - Sehtap Nazlı Kiliç Çeti̇n
 ,
, - Berk Bulut
 ,
, - Halide Gül Okuducu Aydin
 ,
, - Lale Aslanova
 ,
, - Çağdaş Nurettin Emekli̇oğlu
 ,
, - Melike Eren
 ,
, - Elif Uçar
 ,
, - Kaan Eray Uzun
 ,
, - Osman Ufuk Eki̇z
 ,
, - Muhittin Tamer Mungan

Resumo
Original ArticleAnemia levels in the preconception period and the first trimester of pregnancy: a national, multicentric and cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:-e-rbgo1001
DOI 10.61622/rbgo/2025rbgo10001
- Aytaj Jafarzade
 ,
, - Veli Mi̇hmanli
 ,
, - And Yavuz
 ,
, - Murat Akbaş
 ,
, - Gürcan Türkyilmaz
 ,
, - Esra Nur Özkan
 ,
, - Murat İbrahim Toplu
 ,
, - Yücel Kaya
 ,
, - Damla Yasemin Yenli̇k Kaya
 ,
, - Mustafa Yildiz
 ,
, - Ali Emre Ati̇k
 ,
, - Elif İlgazi̇ Kiliç
 ,
, - Burcu Özata
 ,
, - Sehtap Nazlı Kiliç Çeti̇n
 ,
, - Berk Bulut
 ,
, - Halide Gül Okuducu Aydin
 ,
, - Lale Aslanova
 ,
, - Çağdaş Nurettin Emekli̇oğlu
 ,
, - Melike Eren
 ,
, - Elif Uçar
 ,
, - Kaan Eray Uzun
 ,
, - Osman Ufuk Eki̇z
 ,
, - Muhittin Tamer Mungan

Visualizações280Abstract
Objective
The study aimed to determine the level of anemia in pregnant women in the first trimester and in the preconception period by conducting nationwide research.
Methods
The study was designed as retrospective, cross-sectional, and multicenter research. A total of 17 centers from 13 provinces were included in the study. The study was conducted with the participation of two groups of patients who applied to the obstetrics polyclinic between 1 January 2023 and 1 July 2023, who were in the first trimester of pregnancy and who were in the preconception period planning pregnancy.
Results
In total 4,265 women were included in the study. Of these women, 3,884 (91%) were in the first trimester of their pregnancy and 381 (9%) were in the preconception period. Anemia was detected in 24.1% (n=1030) of the patients. Of these patients, 20.6% (n=877) were pregnant women in the first trimester and 3.6% (n=153) were in the preconception period. A statistically significant and positive relationship was found between anemia and meat consumption frequency, educational status, and socioeconomic status of the patients (p=0.000, p=0.000, p=0.000). In addition, a statistically significant and negative correlation was determined between anemia and the number of pregnancies and the parity number (p=0.001, p=0.000) in both groups.
Conclusion
Anemia is a public health problem. Anemia has been determined to be an important problem both in the preconception period and early periods of pregnancy. It is necessary to revise the programs and interventions to reduce the prevalence of anemia and redesign them in line with current conditions.
Palavras-chave: Anemia, iron-deficiencypreconception carePregnancy complications, hematologicPregnancy trimester, firstVer maisVisualizações280

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Resumo
Original ArticleAnemia levels in the preconception period and the first trimester of pregnancy: a national, multicentric and cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:-e-rbgo1001
DOI 10.61622/rbgo/2025rbgo10001
- Aytaj Jafarzade
 ,
, - Veli Mi̇hmanli
 ,
, - And Yavuz
 ,
, - Murat Akbaş
 ,
, - Gürcan Türkyilmaz
 ,
, - Esra Nur Özkan
 ,
, - Murat İbrahim Toplu
 ,
, - Yücel Kaya
 ,
, - Damla Yasemin Yenli̇k Kaya
 ,
, - Mustafa Yildiz
 ,
, - Ali Emre Ati̇k
 ,
, - Elif İlgazi̇ Kiliç
 ,
, - Burcu Özata
 ,
, - Sehtap Nazlı Kiliç Çeti̇n
 ,
, - Berk Bulut
 ,
, - Halide Gül Okuducu Aydin
 ,
, - Lale Aslanova
 ,
, - Çağdaş Nurettin Emekli̇oğlu
 ,
, - Melike Eren
 ,
, - Elif Uçar
 ,
, - Kaan Eray Uzun
 ,
, - Osman Ufuk Eki̇z
 ,
, - Muhittin Tamer Mungan

Visualizações280Abstract
Objective
The study aimed to determine the level of anemia in pregnant women in the first trimester and in the preconception period by conducting nationwide research.
Methods
The study was designed as retrospective, cross-sectional, and multicenter research. A total of 17 centers from 13 provinces were included in the study. The study was conducted with the participation of two groups of patients who applied to the obstetrics polyclinic between 1 January 2023 and 1 July 2023, who were in the first trimester of pregnancy and who were in the preconception period planning pregnancy.
Results
In total 4,265 women were included in the study. Of these women, 3,884 (91%) were in the first trimester of their pregnancy and 381 (9%) were in the preconception period. Anemia was detected in 24.1% (n=1030) of the patients. Of these patients, 20.6% (n=877) were pregnant women in the first trimester and 3.6% (n=153) were in the preconception period. A statistically significant and positive relationship was found between anemia and meat consumption frequency, educational status, and socioeconomic status of the patients (p=0.000, p=0.000, p=0.000). In addition, a statistically significant and negative correlation was determined between anemia and the number of pregnancies and the parity number (p=0.001, p=0.000) in both groups.
Conclusion
Anemia is a public health problem. Anemia has been determined to be an important problem both in the preconception period and early periods of pregnancy. It is necessary to revise the programs and interventions to reduce the prevalence of anemia and redesign them in line with current conditions.
Palavras-chave: Anemia, iron-deficiencypreconception carePregnancy complications, hematologicPregnancy trimester, firstVer mais

This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. 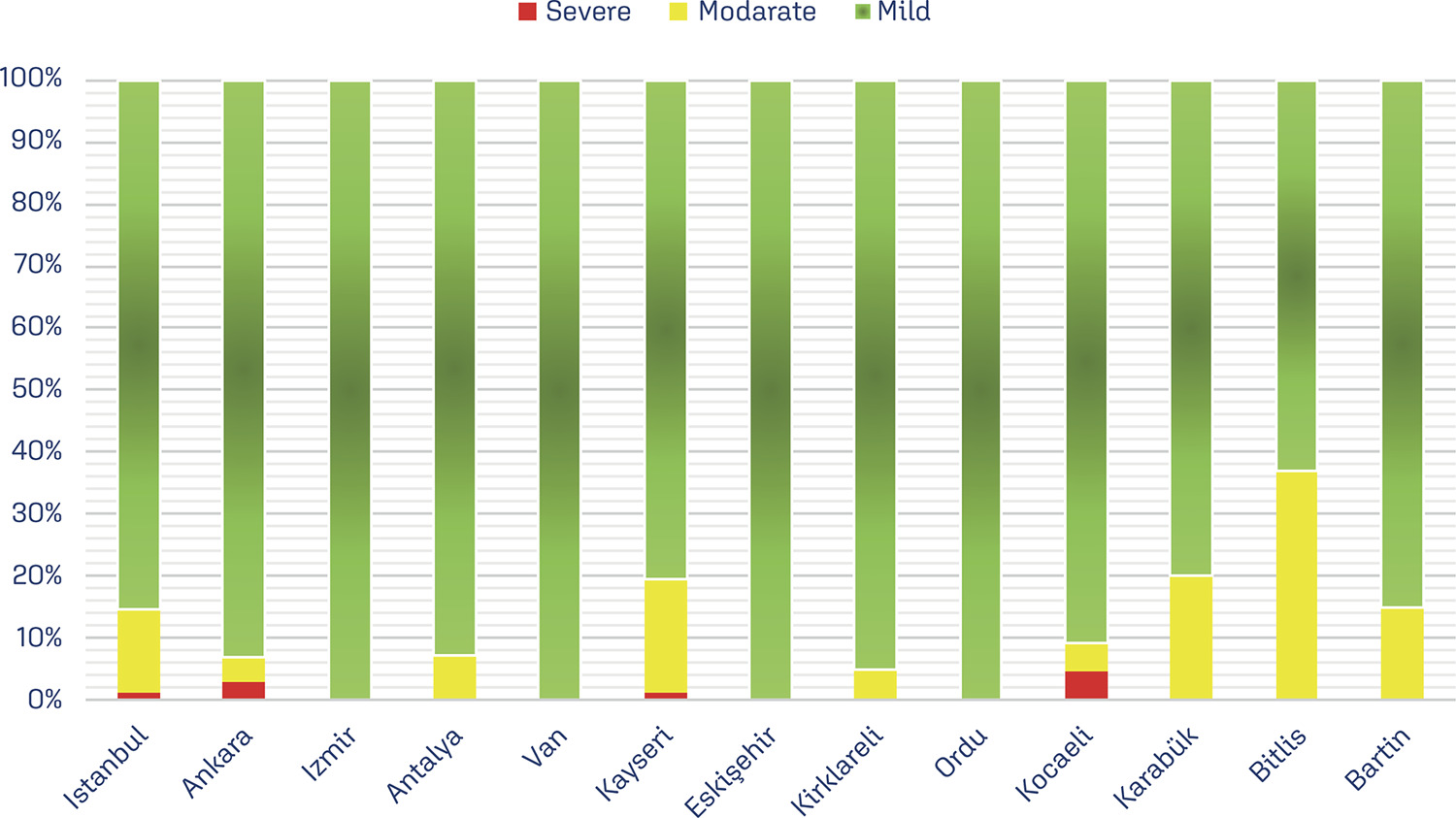
- Aytaj Jafarzade
Objetivos e Visão
A Revista Brasileira de Ginecologia e Obstetrícia (RBGO) tem como objetivo publicar pesquisas básicas e clínicas em ginecologia, obstetrícia e outras especialidades afins e ser referência para apoiar e promover a educação profissional de residentes, pesquisadores e professores universitários. Como VISÃO, a RBGO pretende se tornar uma referência reconhecida internacionalmente entre os principais periódicos mundiais em Ginecologia e Obstetrícia