-
Artigo de Revisão30/04/2025
Letrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
Resumo
Artigo de RevisãoLetrozole and clomiphene versus letrozole alone for ovulation induction in women with PCOS: a systematic review and meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo21
Visualizações168Abstract
Objective:
We aimed to compare the efficacy and safety of letrozole and clomiphene versus letrozole alone for ovulation induction in patients with Polycystic Ovary Syndrome (PCOS).
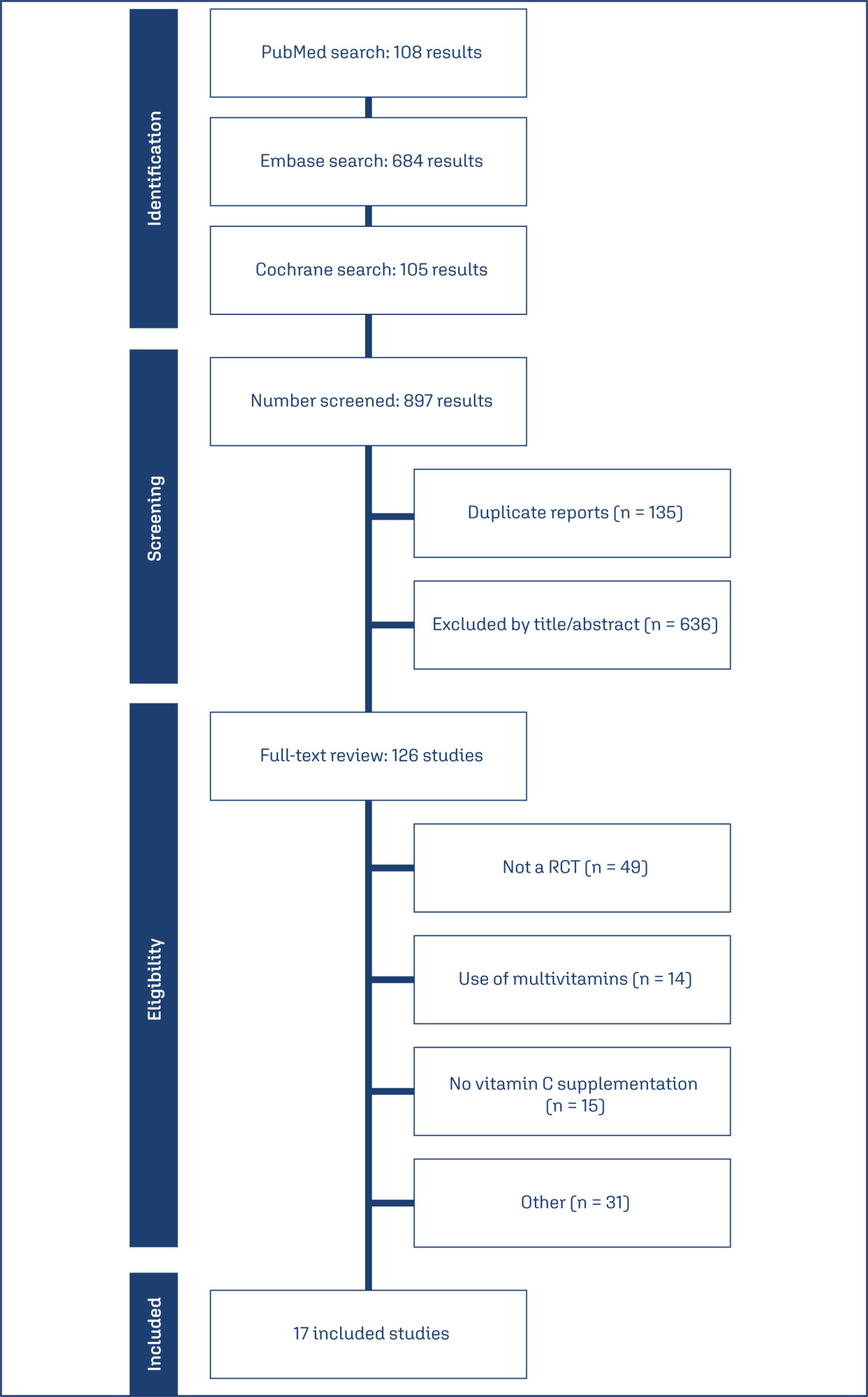
Data Sources:
We systematically searched EMBASE, PubMed, and Cochrane databases on October 31, 2024.
Study selection:
We included studies of women with PCOS treated with a combination of clomiphene and letrozole or letrozole alone to induce ovulation that reported any of the outcomes of interest, namely rate of mature follicles and ovulation, ovulation, pregnancy, miscarriages, endometrial thickness, and number of mature follicles.
Data collection:
We pooled odds ratios (OR) and mean difference (MD) with 95% confidence intervals (CI) using a random effects model using R statistical software, version 4.2.1. Heterogeneity was assessed with I statistics, and a random effects model was used.
Data Synthesis:
Four RCTs and two observational studies comprising 592 patients were included. Combined therapy was associated with a higher rate of a mature follicle (OR 2.74; 95% CI 1.72-4.37; p< 0.001; I=0%) and ovulation (OR 2.55; 95% CI 1.57-4.12; p< 0.001; I=35.9%). The number of mature follicles, number of pregnancies, thickness of endometrial lining, and the incidence of adverse events, including headache, abdominal bloating, fatigue, back pain, breast discomfort, and night sweats, were similar between groups.
Conclusion:
In women with anovulatory infertility secondary to PCOS, letrozole and clomiphene citrate combined therapy was associated with improved mature follicle and ovulation rates, with a similar safety profile compared to letrozole alone. However, no significant impact was observed on pregnancy rates.
Palavras-chave: ClomipheneInfertility, femaleLetrozoleOvulationOvulation InductionPolycystic ovary syndromeVer mais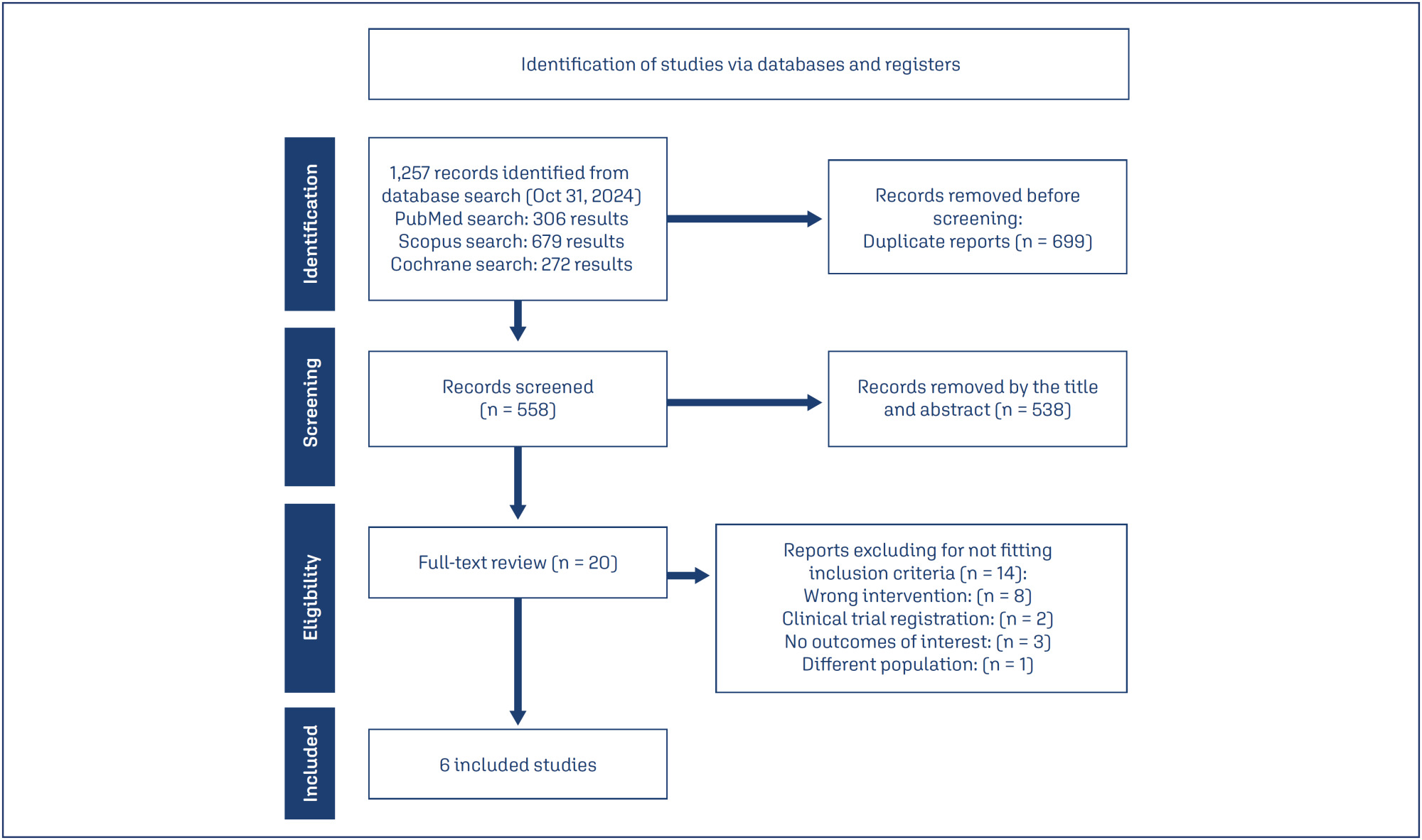
-
Artigo Original30/04/2025
Incidence of small-for-gestational-age newborns in pregnant women with COVID-19
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo20
Resumo
Artigo OriginalIncidence of small-for-gestational-age newborns in pregnant women with COVID-19
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo20
Visualizações138Abstract
Objective:
This study aimed to assess the incidence of small for gestational age (SGA) newborns in pregnant women infected with COVID-19 and examine the associated neonatal outcomes.
Methods:
This study involved a secondary analysis of the REBRACO Network, a prospective cohort study conducted in 15 maternity hospitals in Brazil before the introduction of COVID-19 vaccination (February 2020 to February 2021). Demographic data of pregnant women tested for COVID-19 were analyzed, and fetal outcomes were compared between women with positive and negative COVID-19 results who had SGA fetuses.
Results:
A total of 729 symptomatic pregnant women with COVID-19 were included in the study. However, there were 248 participants with missing information regarding childbirth or loss of follow-up, and 107 participants without confirmatory tests for COVID-19. Among the remaining participants, 198 had confirmed COVID-19 and 176 tested negative. The incidence of SGA among women with COVID-19 was 22.4%, whereas the incidence among women who tested negative for COVID-19 was 14.8%. SGA newborns born to COVID-19 positive pregnant women were 1.6 times more likely to experience adverse outcomes (such as prematurity, stillbirth, neonatal death, and admission to a neonatal ICU) compared to non-SGA newborns [OR = 1.655 (1.145 – 2.394); P=0.017]. In SGA newborns of pregnant women with confirmed COVID-19 infection, mechanical ventilation use was found to be associated with the infection [OR = 0.692 (0.562 – 0.853); P=0.002].
Conclusion:
The higher incidence of SGA newborns and its stronger association with prematurity in pregnant women with confirmed COVID-19 infection suggest that COVID-19 infection is a significant factor contributing to neonatal morbidity and mortality.
Palavras-chave: coronavirus infectionsCOVID-19Infant, newbornInfant, small for gestational agematernal healthPregnancy complicationsVer mais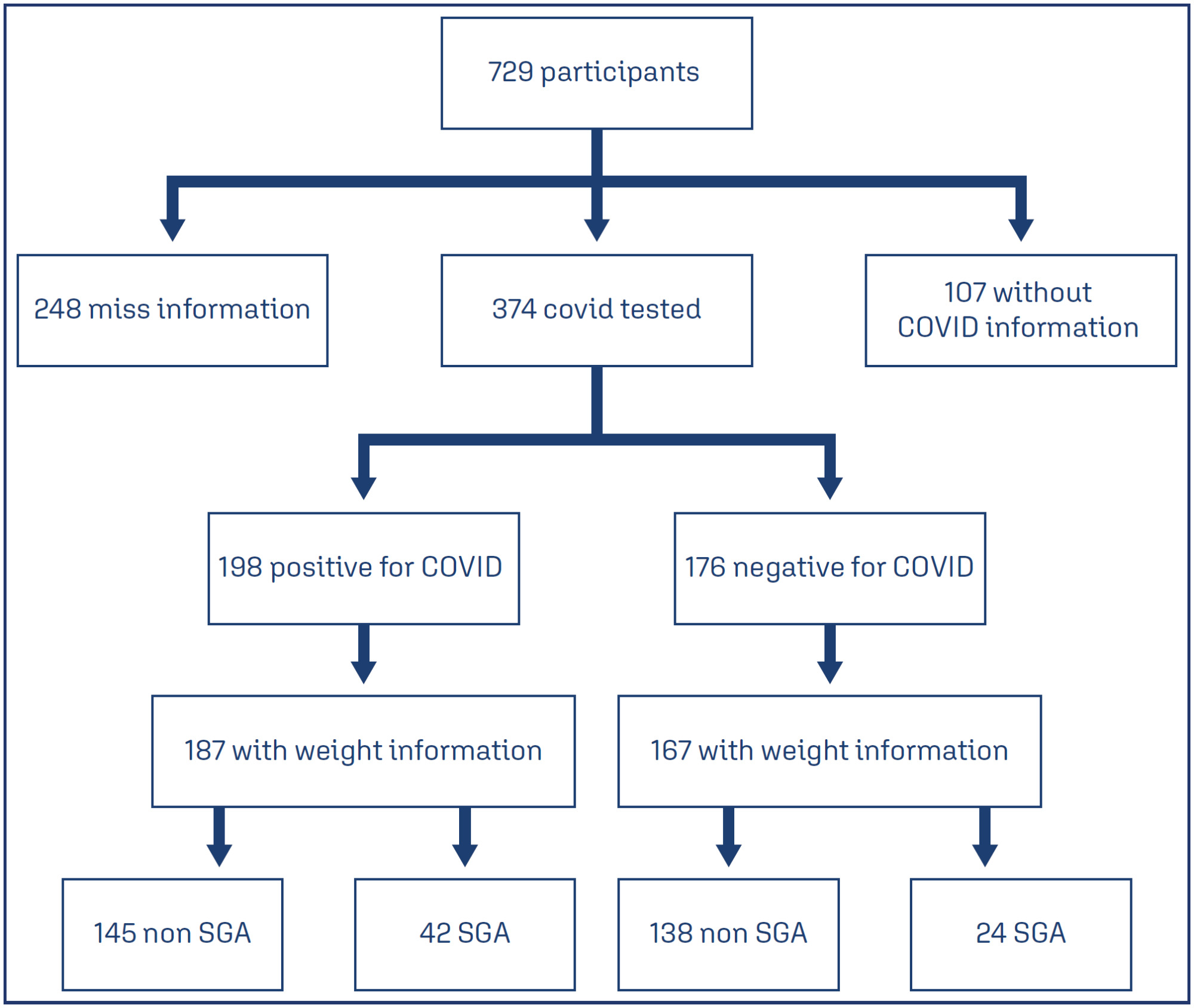
-
Artigo de Revisão30/04/2025
Efficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo18
Resumo
Artigo de RevisãoEfficacy of tranexamic acid application in gynecology and obstetrics procedures: a umbrella review of systematic reviews of randomized trials
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo18
Visualizações143Abstract
Objective:
This umbrella review aimed to synthesize evidence from systematic reviews of clinical trials on the efficacy of tranexamic acid in gynecology and obstetrics procedures.
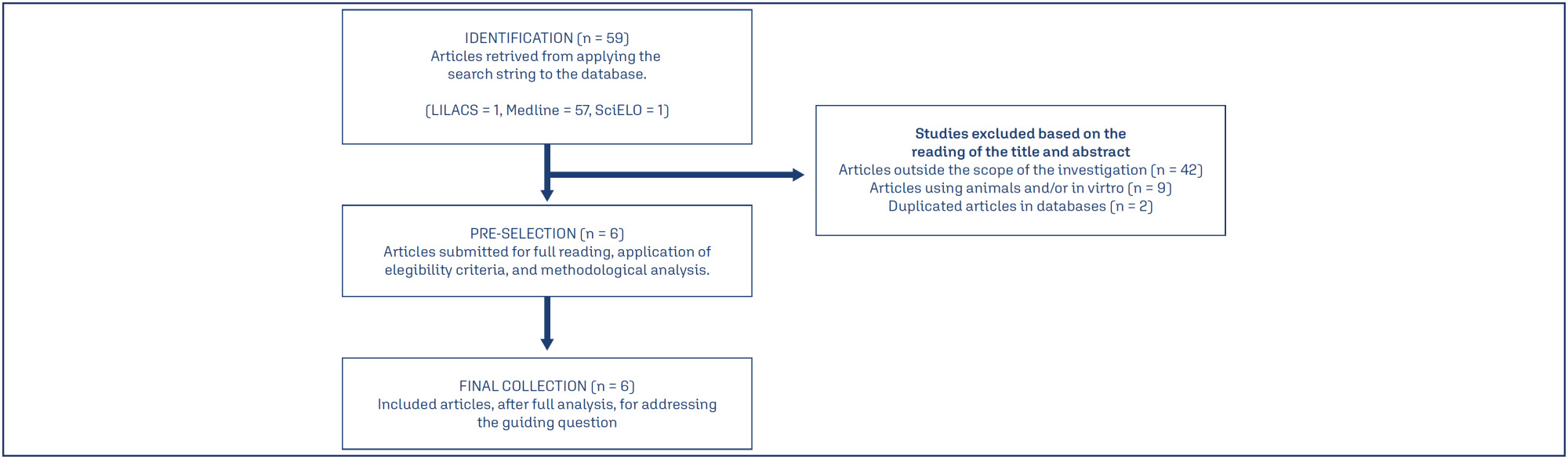
Methods:
We searched Medline, Embase, SciELO and Cochrane Database of Systematic Reviews on March 11, 2024, using the term “tranexamic acid”. Four reviewers independently select studies and extract data. We assessed the quality of systematic review and the quality of evidence, using AMSTAR 2 and GRADE tools, respectively.
Results:
Of 651 systematic reviews identified, 16 reviews with 96663 patients were included. The surgical procedures were cesarean section, myomectomy, hysterectomy, and cervical intraepithelial neoplasia surgery. All reviews showed a statistically significant and clinically relevant reduction in intraoperative and post-procedure blood loss, associated with intravenous or topical use of tranexamic acid. Tranexamic acid resulted in a significant reduction in the need for blood transfusions and a less pronounced drop in postoperative hematocrit and hemoglobin levels in cesarean section. Several reviews addressed the same question, but the number of included trials varied substantially, which might indicate flaws in search and selection of studies of these reviews. The quality of systematic reviews was low or critically low, and the quality of evidence was moderate.
Conclusions:
This umbrella review shows that tranexamic acid can reduce blood loss and hemorrhage in gynecology and obstetrics procedures. High quality systematic reviews are still needed.
Palavras-chave: Blood transfusionCesarean sectionEfficacyGynecologic surgical procedureshematocritHemorrhageHysterectomyObstetric surgical proceduresTranexamic acidUterine cervical dysplasiauterine myomectomyVer mais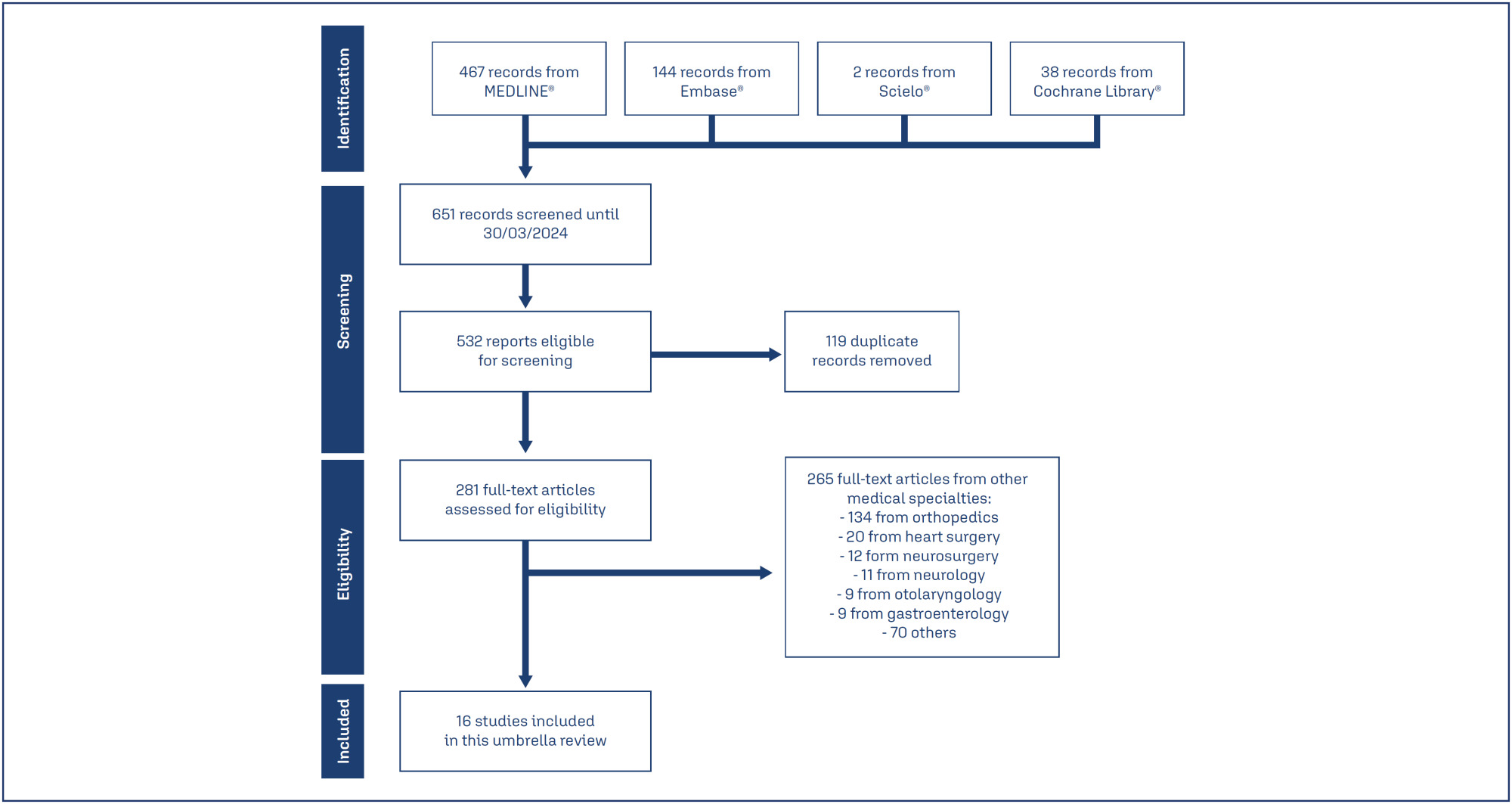
-
Artigo Original30/04/2025
Assessıng the predıctıve accuracy of blood-based bıomarkers ın neonatal outcomes for pregestatıonal dıabetes mellıtus
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo17
Resumo
Artigo OriginalAssessıng the predıctıve accuracy of blood-based bıomarkers ın neonatal outcomes for pregestatıonal dıabetes mellıtus
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo17
Visualizações125Abstract
Objective:
This retrospective study aimed to investigate blood-based immune-inflammatory biomarkers (IIBs) in predicting neonatal outcomes in pregnancies with pregestational diabetes mellitus (PGDM).PIV[(neutrophil×platelet×monocyte)/lymphocyte)], SII (neutrophil×platelet/lymphocyte), and NLR neutrophil/lymphocyte) values were evaluated in all three trimesters, and their correlation with neonatal outcomes was examined.
Methods:
We included 82 cases of PGDM pregnancies delivered after 32 weeks. Maternal age, gravidity, parity, types of diabetes, and route of delivery were noted. For neonatal outcomes, we recorded gestational age at birth, birth weight percentile, existence of fetal growth restriction, LGA, neonatal intensive care unit (NICU) requirement, Apgar Score <7 at 1, 5, or 10 minutes, need for positive pressure ventilation (PPV), need for mechanical ventilation, hypoglycaemia, hyperbilirubinemia and the need for phototherapy. PIV, SII and NLR values were calculated in each trimester and their association with adverse neonatal outcomes was analyzed.
Results:
We could not detect any consistent and significant correlation between SII and PIV values and adverse neonatal outcomes for each trimester. There was a correlation between 3rd trimester NLR and adverse neonatal outcomes, including APGAR <7, the requirement for PPV and mechanical ventilation (p=0.056, 0.013 and 0.060, respectively).
Conclusion:
While SII and PIV values did not consistently correlate with adverse neonatal outcomes throughout each trimester in PGDM pregnancies, 3rd-trimester NLR showed a notable association with the requirement for PPV with statistical significance and with Apgar Score <7 and the requirement for mechanical ventilation without statistical significance. NLR in the third trimester may hold potential as a predictive marker for specific adverse neonatal outcomes in PGDM pregnancies, warranting further investigation.
Palavras-chave: biomarkersDiabetes mellitusGestational ageHypoglycemiaInfant, newbornIntensive care units, neonatalLymphocytesMaternal ageMonocytesNeuthrophilsPregancyPregnancy in diabetesRespiration, artificialVer mais -
Artigo Original30/04/2025
Effects of domestic violence on menopausal symptoms, sexual function, and quality of life: a cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo16
Resumo
Artigo OriginalEffects of domestic violence on menopausal symptoms, sexual function, and quality of life: a cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo16
Visualizações127Abstract
Objective:
To investigate the association between lifetime experience of domestic violence and climacteric symptoms, sexual function, and quality of life in climacteric women in Rio Grande do Sul, Brazil.
Methods:
A cross-sectional study was conducted with 700 pre-, peri-, and postmenopausal women, recruited online via an anonymous questionnaire (REDCap platform). Women aged 40 to 65 years, residing in Rio Grande do Sul, and classified by the STRAW+10 criteria were included. Climacteric symptoms and sexual function were assessed using the 10-item Cervantes Scale (CS-10) and the 6-item Female Sexual Function Index (FSFI-6). Data were analyzed using SPSS version 18.0; quantitative data as median [IQR], qualitative as frequencies. Group comparisons used Kruskal-Wallis, Chi-Square, and Spearman’s correlation between violence against women (VAW) and/or climacteric groups on CS-10 or FSFI-6. Significance was set at 5%.
Results:
The median [IQR] age of pre- (46 [43 – 50] years), peri- (50 [47 – 52] years), and postmenopausal (55 [51 – 58] years) were different among groups. Prevalence rates of psychological (38.8%), sexual (34.9%), and physical (21.3%) violence were observed. Postmenopausal women showed the poorest outcomes. Premenopausal women experiencing violence had severe anxiety, while postmenopausal women reported feeling worthless. Various sexual dysfunctions were associated with violence, including low desire, lubrication issues, and sexual pain.
Conclusions:
Domestic violence was linked to worse climacteric symptoms, sexual function, and quality of life, particularly in postmenopausal women. These findings underscore the need for improved care and public policies to enhance safety and well-being among women of all ages.
Palavras-chave: AnxietyClimactericDomestic violenceMenopausePostmenopauseQuality of lifeSexualitysurveys and questionnairesViolence against womenVer mais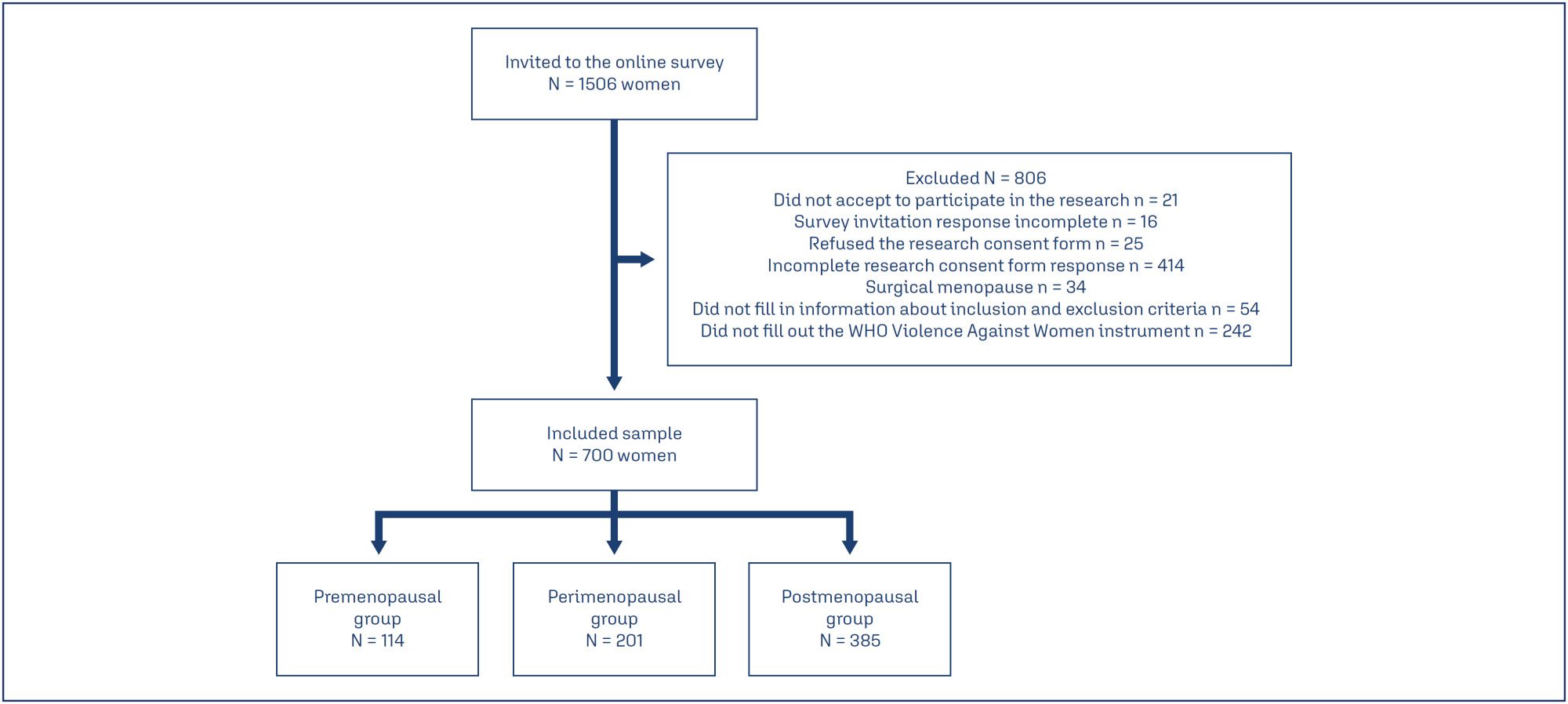
-
Artigo Original30/04/2025
The ımpact of demographic and obstetric factors on perception of traumatic birth and breastfeeding attitudes
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo15
Resumo
Artigo OriginalThe ımpact of demographic and obstetric factors on perception of traumatic birth and breastfeeding attitudes
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo15
Visualizações93Abstract
Objective:
This study aims to examine the effects of sociodemographic and obstetric factors on traumatic birth perception and breastfeeding attitudes in primiparous mothers who have had a vaginal birth in the early postpartum period.
Methods:
The sample of the research, developed with a cross-sectional and correlational design, consisted of 252 women residing in a province in the Western Black Sea region of Türkiye. The data were obtained by employing a Personal Information Form, Traumatic Childbirth Perception Scale, and Breastfeeding Attitudes of The Evaluation Scale. Data analysis was conducted using the statistical programming language R (R version 4.3.3).
Results:
Women who were not employed, had a planned pregnancy, and did not experience health problems during pregnancy had higher mean breastfeeding attitude scores, and this difference was statistically significant. It was determined that a one-unit increase in gestational week led to an average increase of 1.926 units in breastfeeding attitude score, and a one-unit increase in Traumatic Childbirth Perception Scale score led to an average decrease of 0.110 units in breastfeeding attitude score. The mean traumatic childbirth perception scores of women living in urban areas were found to be lower than those living in villages or towns, and the difference was statistically significant.
Conclusion:
The research findings indicate that gestational age, perception of traumatic childbirth, and certain sociodemographic factors significantly affect breastfeeding attitudes. Additionally, mothers living in urban areas have a lower perception of traumatic childbirth. Therefore, individualized approaches to childbirth and breastfeeding support are crucial.
Palavras-chave: Breast feedingDelivery, obstetricParturitionperceptionPostpartum periodSociodemographic factorsStress disorders, post-traumaticVer mais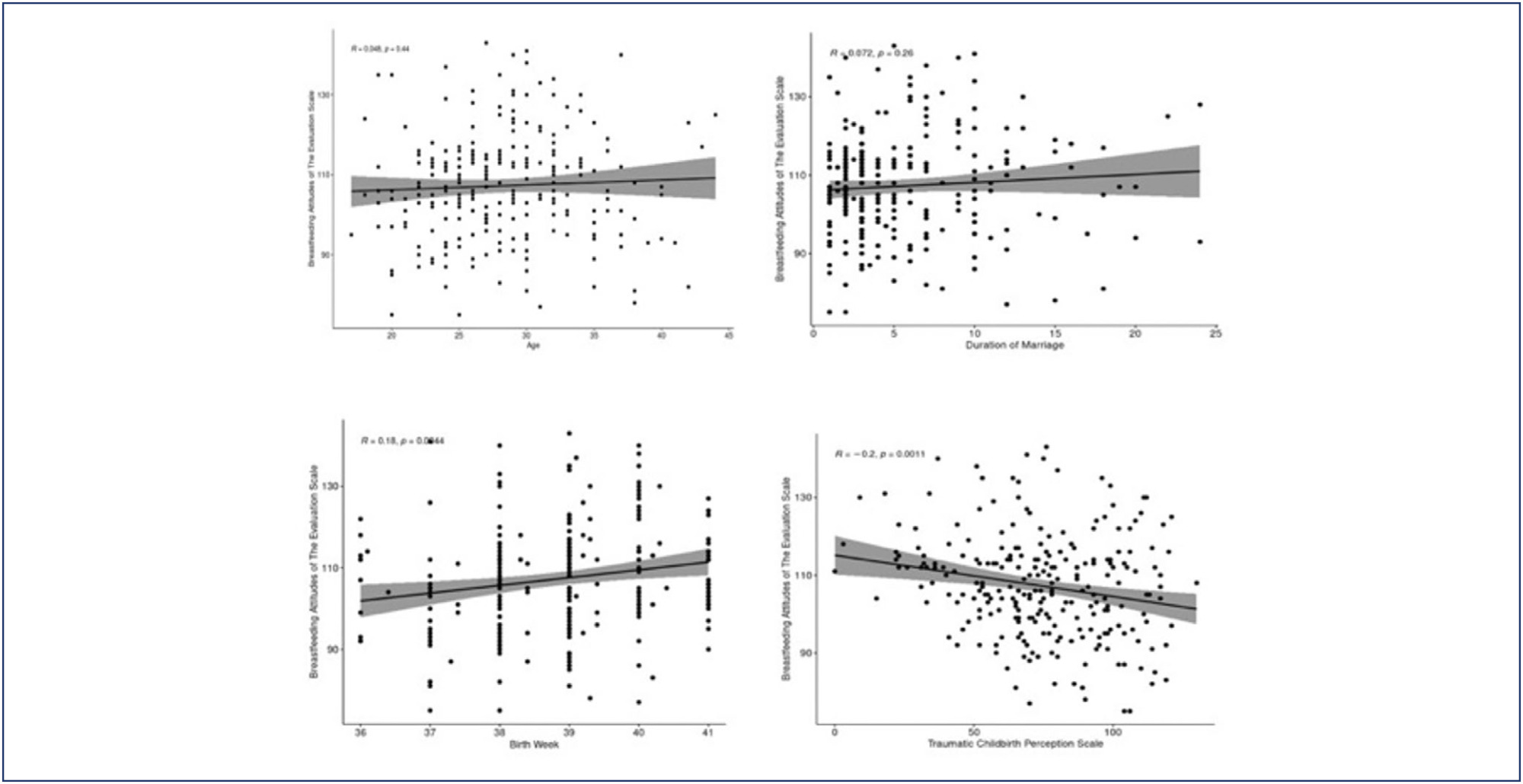
-
Artigo Original30/04/2025
Clinical and epidemiological profile of pregnant and postpartum women affected by COVID-19 who required respiratory support
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo14
Resumo
Artigo OriginalClinical and epidemiological profile of pregnant and postpartum women affected by COVID-19 who required respiratory support
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo14
Visualizações100Abstract
Objective:
This study described the clinical and epidemiological profile and the management provided to pregnant and postpartum women with COVID-19 who required respiratory support.
Methods:
A descriptive study was conducted with pregnant and postpartum women with confirmed COVID-19 who received care between April 2020 and December 2021 in eight referral centers in northeastern Brazil. Statistical analysis was conducted using Epi-Info 7.2.5 and Medcalc, version 20.112.
Results:
Of the 720 patients admitted, 208 (32.7%) required respiratory support. Mean age of the participants was 28.9±7.1 years. Most (52.8%) were brown-skinned; 31.3% had little formal schooling; 41.1% had a personal income and 23.1% were married. Around half were referred from another hospital. Overall, 36.8% were obese and 36.9% were hypertensive. Criteria for severe acute respiratory syndrome (SARS) were present in 80.7% of cases. Overall, 151 patients (74.7%) required corticoids, and 150 (76.1%) were admitted to an intensive care unit. Non-invasive ventilation was needed in 89.4% of cases, with nasal catheters being the most common type (55.3% of cases). Invasive mechanical ventilation was necessary in 35.5% of cases and 91.6% had a cesarean section. Maternal near miss and death occurred in 24% and 12.9% of cases, respectively.
Conclusion:
Pregnant and postpartum women with COVID-19 who required respiratory support were predominantly brown-skinned, in the third trimester of pregnancy and had been referred from another hospital. The cesarean section rate was high; the presence of criteria for SARS was common and the rates of COVID-19-related maternal near miss and death were high.
Clinical Trials registry:
NCT04462367
Palavras-chave: Cesarian sectionCOVID-19Intensive care unitsNear miss, healthcareNoninvasive ventilationObesityPostpartum periodPregnancyPregnancy trimester, thirdRespiration, artificialSARS-CoV-2severe acute respiratory syndromeVer mais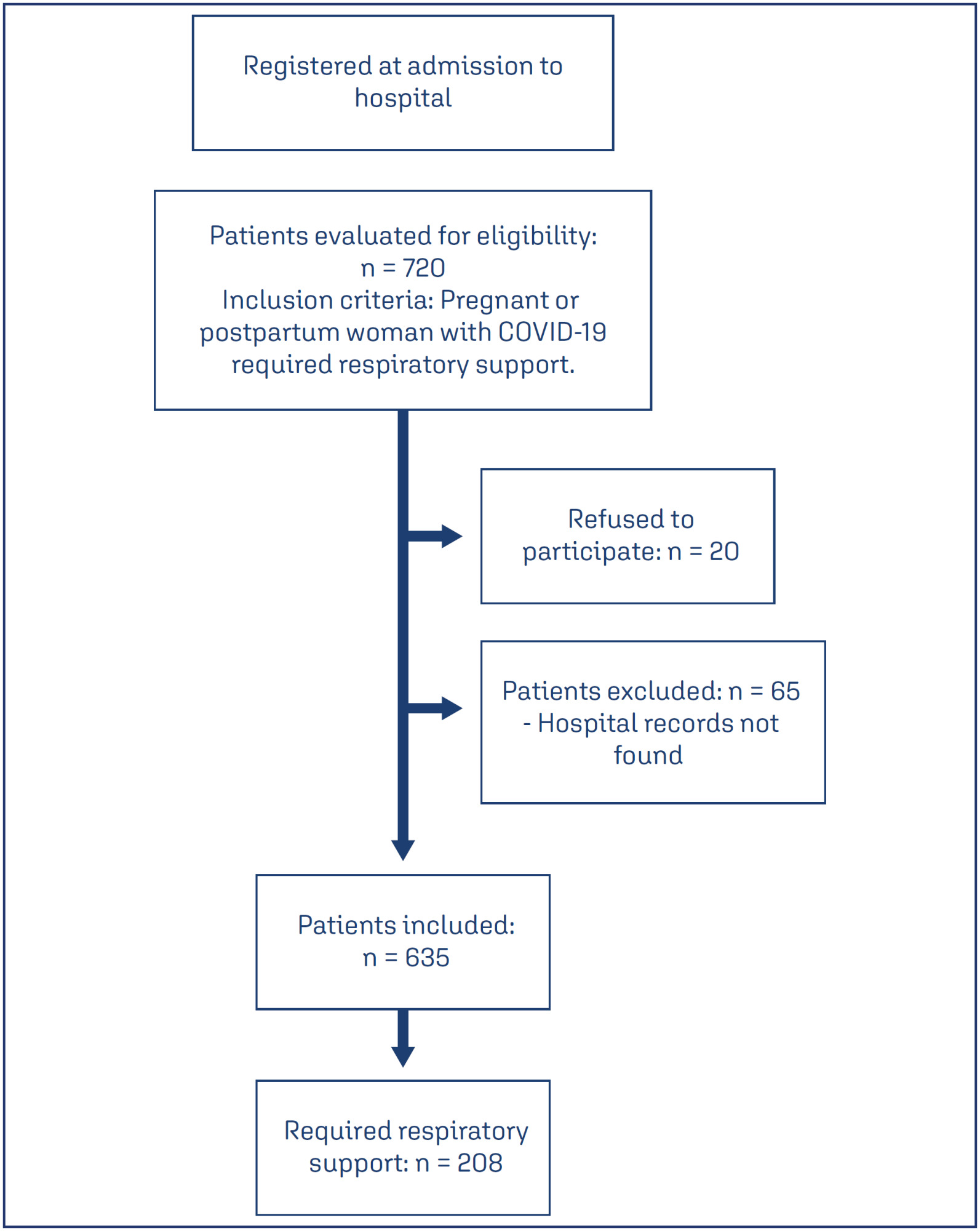
-
Artigo Original30/04/2025
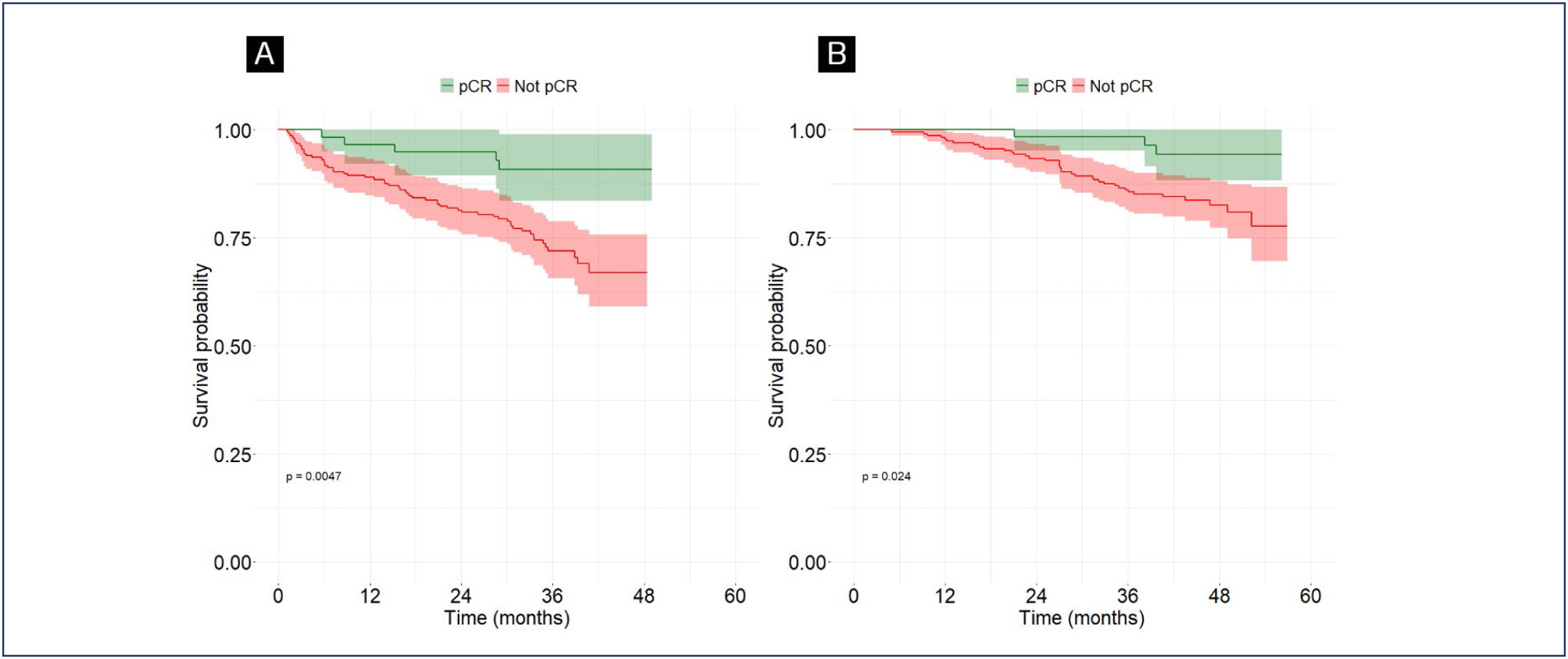
Evaluation of pathological complete response rates in breast cancer patients undergoing neoadjuvant therapy
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo13
Resumo
Artigo OriginalEvaluation of pathological complete response rates in breast cancer patients undergoing neoadjuvant therapy
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo13
Visualizações111Ver maisAbstract
Objective:
This study aims to assess the rate of pathological complete response (pCR) in breast cancer patients undergoing neoadjuvant therapy and to explore its correlation with clinical, molecular, and prognostic factors.
Methods:
We conducted this retrospective observational study at Liga Contra o Câncer, a major public oncology reference center in Northeast Brazil. We included patients diagnosed with breast cancer who initiated neoadjuvant therapy between June 2018 and June 2019. Patients with a history of recurrent breast cancer or those who did not undergo surgery were excluded. The primary outcome was the pCR rate, with secondary outcomes including Overall Survival (OS), Disease-Free Survival (DFS), mortality, and disease recurrence. Follow-up extended until August 2022. We performed multivariate Cox regression analysis to correlate outcomes with predetermined variables.
Results:
Of the 292 included patients, 63 (21.6%) achieved pCR. The mean follow-up duration was 42.8 months. Multivariate logistic regression analysis revealed an association between pCR and the AC-TH regimen [OR = 2.4; 95%CI = 1.13 – 5.24; p=0.023], as well as between pCR and HER2-positive tumors [OR 2.49; 95% CI = 1.14 – 5.86; p=0.028]. Complete pathological response was associated with higher DFS [HR 0.33; 95%CI 0.13-0.86; p=0.024].
Conclusion:
Neoadjuvant therapy demonstrated significant efficacy in achieving pathological response in breast cancer patients. We observed a strong association between the AC-TH regimen, HER2-positive status, and pCR.
Busca
Pesquisar em:
Nuvem de Tags
Gravidez (167)Fatores de risco (89)Menopausa (79)Pré-eclâmpsia (66)Endometriose (65)Mama (59)Infertilidade (58)Obesidade (57)Complicações na gravidez (56)Diagnóstico pré-natal (54)Gestação (54)Qualidade de vida (53)Saúde da mulher (51)Cesárea (50)Complicações da gravidez (50)Neoplasias da mama (49)Fertilização in vitro (48)Cuidado pré-natal (47)Mortalidade materna (43)Ultra-sonografia (43)