Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):796-807
Menopause causes several changes in the body that may affect the response to COVID-19. We aimed to investigate the possible association between menopausal status and incidence and outcomes in COVID-19 patients.
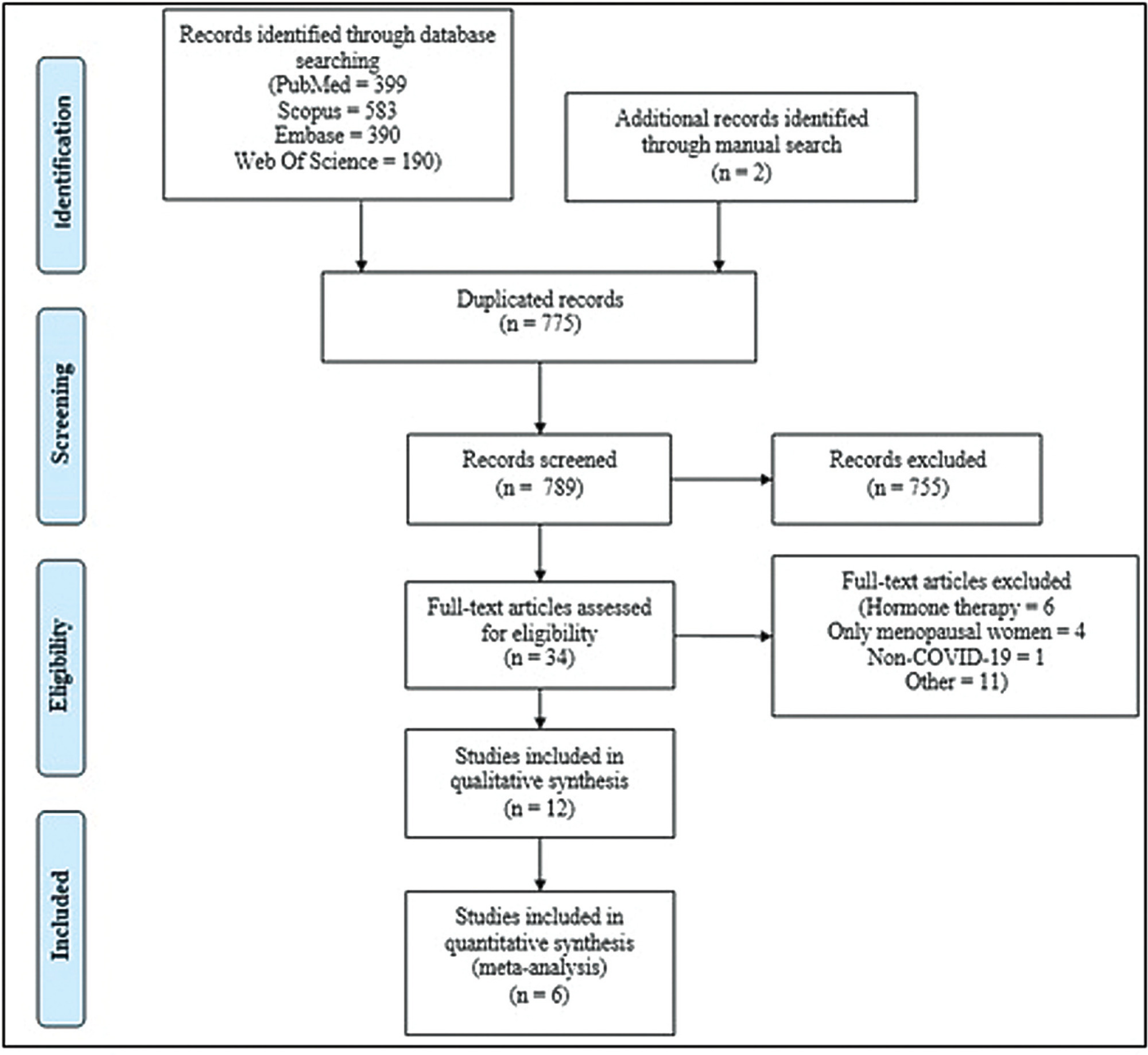
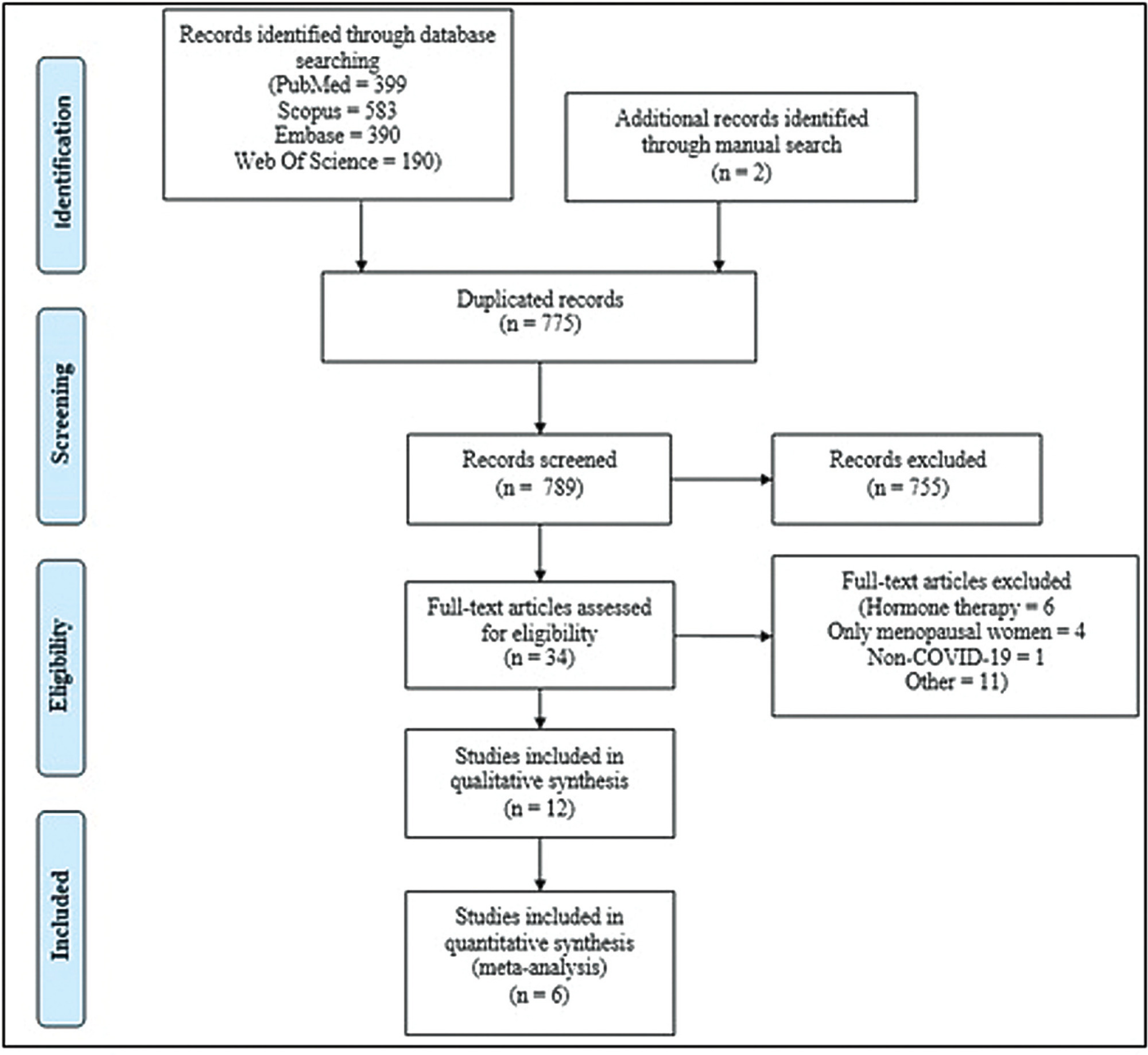
Combinations of keywordsCOVID-19, menopause, and estrogen were used to search the PubMed, Embase, Web-of-Science, and Scopus databases for articles reporting the incidence and outcomes of COVID-19 (discharge, length-of-admission, intensive care, or mortality) in premenopausal women, available through December 29, 2022. Data from studies comparing the incidence of COVID-19 infection with the age-matched male population were pooled and meta-analyzed using a random-effects model.
Overall, 1,564 studies were retrieved, of which 12 were finally included in the systematic review to compare disease outcomes, and 6 were meta-analyzed for the incidence of COVID-19 in premenopausal and postmenopausal women. All studies reported better COVID-19-associated outcomes in premenopausal women compared with postmenopausal women. After adjusting for confounding factors, three studies found better outcomes in postmenopausal women, and two found no association between menopausal status and COVID-19 outcomes. Our meta-analysis found a higher incidence of COVID-19 infection among premenopausal women than postmenopausal women, when compared with age-matched men (odds ratio = 1.270; 95% confidence interval: 1.086–1.486; p = 0.003).
The incidence of COVID-19 was significantly higher in premenopausal women than in postmenopausal women when compared with age-matched men. Although premenopausal women may have more favorable COVID-19-associated outcomes, the presumed preventive effect of estrogens on the incidence and related outcomes of COVID-19 in premenopausal women cannot be proven at present. Further longitudinal studies comparing pre- and post-menopausal women are required to provide further insight into this matter.
Search
Search in:

Comments