Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(1):46-53
Magnetic resonance imaging (MRI) has been considered another tool for use during the pre- and postoperative periods of the management of pelvic-organ prolapse (POP). However, there is little consensus regarding its practical use for POP and the association betweenMRI lines of reference and physical examination.We aimedto evaluate the mid- to long-term results of two surgical techniques for apical prolapse.
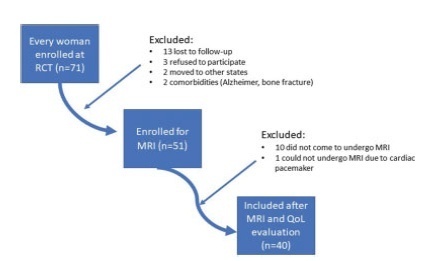
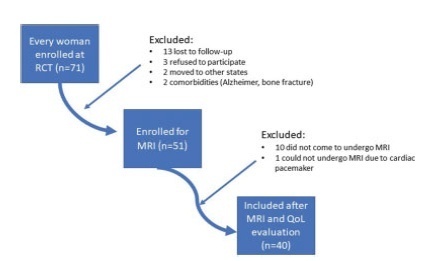
In total, 40 women with apical POP randomized from 2014 to 2016 underwent abdominal sacrocolpopexy (ASC group; n = 20) or bilateral vaginal sacrospinous fixation with an anterior mesh (VSF-AM group; n = 20). A physical examination using the POP Quantification System (POP-Q) for staging (objective cure) and the International Consultation on Incontinence Questionnaire-Vaginal Symptoms (ICIQ-VS: subjective cure), were applied and analyzed before and one year after surgery respectively. All MRI variables (pubococcigeous line [PCL], bladder base [BB], anorectal junction [ARJ], and the estimated levator ani subtended volume [eLASV]) were investigated one year after surgery. Significance was established at p < 0.05.
After a mean 27-month follow-up, according to the MRI criteria, 60% of the women were cured in the VSF-AM group versus 45% in ASC group (p= 0.52). The POP-Q and objective cure rates by MRI were correlated in the anterior vaginal wall (p= 0.007), but no correlationwas foundwith the subjective cure. The eLASVwas largeramongthe patients with surgical failure, and a cutoff of ≥ 33.5mm3 was associated with postoperative failure (area under the receiver operating characteristic curve [ROC]: 0.813; p= 0.002).
Both surgeries for prolapse were similar regarding theobjective variables (POP-Q measurements and MRI cure rates). Larger eLASV areas were associated with surgical failure.
Search
Search in:

Comments