Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(12):800-804
In recent years, there has been an increase in the incidence of ectopic pregnancies; therefore, it is important for tertiary centers to report their approaches and outcomes to expand and improve treatment modalities. The aim of the present study was to evaluate the general characteristics, treatment and outcomes of cases diagnosed with ectopic pregnancy.
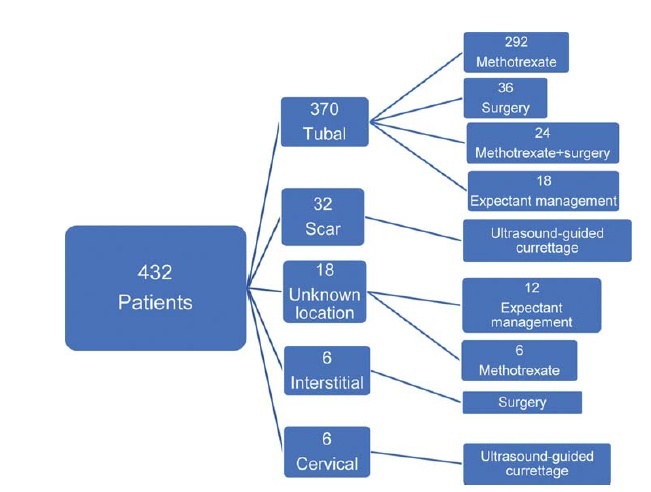
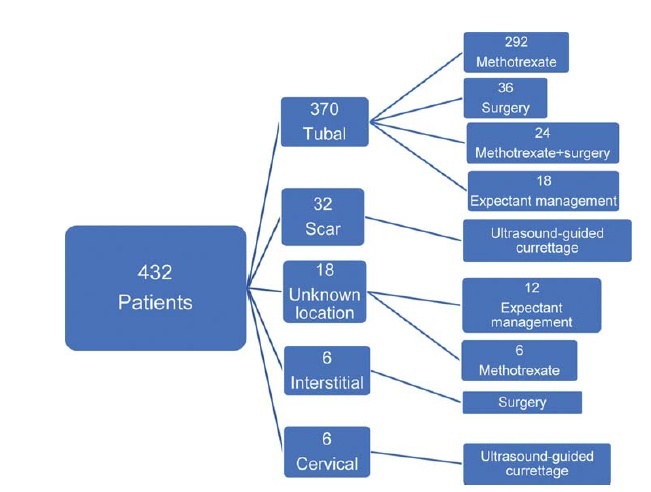
In total, 432 patients treated for ectopic pregnancy between February 2016 and June 2019 were retrospectively evaluated.
Overall, 370 patients had tubal pregnancy, 32 had cesarean scar pregnancy, 18 had pregnancy of unknown location, 6 had cervical pregnancy, and 6 had interstitial pregnancy. The most important risk factors were advanced age (> 35 years; prevalence: 31.2%) and smoking (prevalence: 27.1%). Thirty patients who did not have any symptoms of rupture and whose human chorionic gonadotropin (β-hCG) levels were ≤ 200 mIU/ml were followed-up with expectant management, while 316 patients whose β-hCG levels were between 1,500 mIU/ml and 5,000 mIU/ml did not have an intrauterine gestational sac on the transvaginal or abdominal ultrasound, did not demonstrate findings of rupture, and were treated with a systemic multi-dose methotrexate treatment protocol. In total, 24 patients who did not respond to the medical treatment, 20 patients whose β-hCG levels were > 5,000 mIU/ml, 16 patients who had shown symptoms of rupture at the initial presentation, and 6 patients diagnosed with interstitial pregnancy underwent surgery. Patients with cervical and scar pregnancies underwent ultrasound-guided curettage, and no additional treatment was needed.
The fertility status of the patients, the clinical and laboratory findings, and the levels of β-hCG are the factors that must be considered in planning the appropriate treatment.
Search
Search in:

Comments