Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(4):317-323
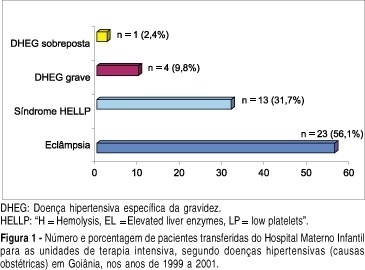
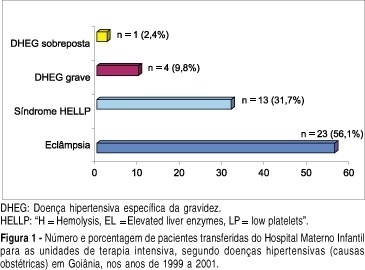
OBJECTIVE: to evaluate the epidemiological and parturitional aspects of obstetric patients admitted to intensive care units (ICU), and analyze the frequency of intensive support needed by them. METHODS: observational and descriptive study of all obstetric patients’ transfers to ICU from the Hospital Materno Infantil of Goiânia-Go, from January 1999 to December 2001. The analysis has included variables as maternal age, parity, obstetric and non-obstetric indications for ICU admissions, moment of transfer, mode of delivery, maternal death, and the frequency of ICU utilization per 1,000 deliveries (IDR – imminent death ratio). The statistical analysis was performed by the chi2 test or the Fisher exact test and a significant difference was set at a level of 5%. RESULTS: over the 36-month period analyzed, 86 pregnancy-associated ICU admissions were identified (among 4,560 deliveries). Of the 86 patients, 52.33% (n=45) were nulliparae and 63 (73.26%) were between 19 and 35 years old. Hypertensive disorders accounted for 41 (57.75%) of the admissions and hemorrhage for 14 (19.72%). Eclampsia (n=23), HELLP syndrome (n=13) and premature abruptio placentae (n=5) were the most common obstetric indications for ICU admissions. Maternal cardiac disorders accounted for 4 cases of non-obstetric indications. There was a predominance of postpartum transfers (82.35%). Fifty-five (72.37%) patients needed delivery by caesarian section. The average time spent in the UCI by those patients was 5.1 days. Maternal mortality found in this study was 24.29%, hypertensive disorders being responsible for 52.94% (9/17) of all obstetric-associated deaths. There were no significant statistical differences (p=0.81) regarding these obstetric-associated deaths and their causes (hypertensive disorders, hemorrhage or infections) or even regarding maternal deaths and duration of stay (< or > 48 hours) in the ICU (p=0.08). The IDR found was 18.8 per 1,000 deliveries. CONCLUSIONS: the need of intensive care estimated by IDR was 18.8 per 1,000 deliveries, the pregnancy-induced hypertension being responsible for the majority of the indications for maternal transfers.
Search
Search in:

Comments