Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(10):485-491
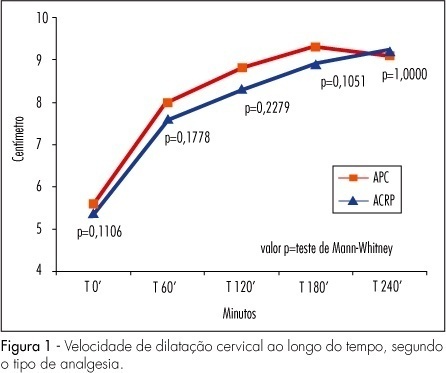
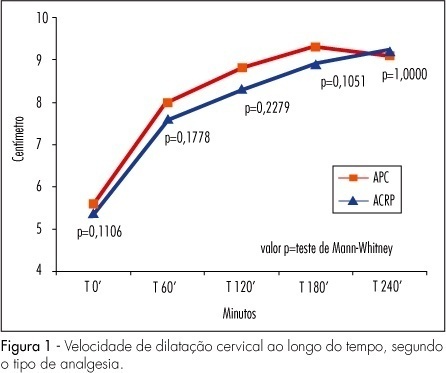
PURPOSE: to compare maternal and perinatal results, after the use of continuous peridural versus combined rachidian and peridural analgesia in primiparous parturients. METHODS: randomized clinical trial with 128 primiparous pregnant women in labor, divided into two groups: peridural analgesia (CPA) with 65 women, and combined continuous rachidian and peridural analgesia (CRPA) with 63, all of them admitted in the pre-labor period at two maternities in Jundiai, in the state of São Paulo. The variables studied were: latency of analgesia onset, pain intensity, total time until complete dilation, Apgar index at the first and fifth minutes, labor duration, degree of motor blockade, adverse effects such as vomiting, pruritus, arterial hypotension and degree of maternal fulfillment. Inclusion criteria were: primiparous, physical condition ASA 1 and 2, an only foetus, cephalic presentation, term delivery, 3 to 6 cm cervical dilation, and analgesia required by the obstetritian. Women with morbidity, membrane rupture, fetal abnormality and use of opioids up to four hours before were excluded. The Mann-Whitney test was used for the statistical analysis of non-parametric continuous variables, and Fisher’s exact and Pearson’s χ2 tests, for the categoric variables. RESULTS: there was no difference between the groups concerning the length of cervical dilation, labor duration, maternal hemodynamic parameters, newborn vitality, analgesic complementation during labor and type of delivery. Analgesia onset was quicker in the CRPA group, and the CPA group presented less motor blockade. Differences concerning adverse effects such as nausea, vomiting, pruritus and hypotension have not been observed, but hypotension was more frequent in the CPA group (6.3 versus 3.1%). CONCLUSIONS: both techniques have proved to be safe and efficient, but CRP has provided an earlier onset, with quicker pain relief. The lesser motor blockade in the CPA group has allowed the parturients more active movements in bed and more effective collaboration during the expulsion period. Most women were pleased with the analgesia they got. The doses of local anesthetics and opioids used in both analgesic techniques and the complementary doses, equal in both groups, neither had any significant adverse effect nor affected newborn vitality.
Search
Search in:

Comments