Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):560-566
To identify the barriers to provide to women and adequately train physicians on therapeutic abortions in public hospitals in Peru.
Descriptive cross-sectional survey-based study. We invited 400 obstetrics and gynecology specialists from 7 academic public hospitals in Lima and 8 from other regions of Peru. Expert judges validated the survey.
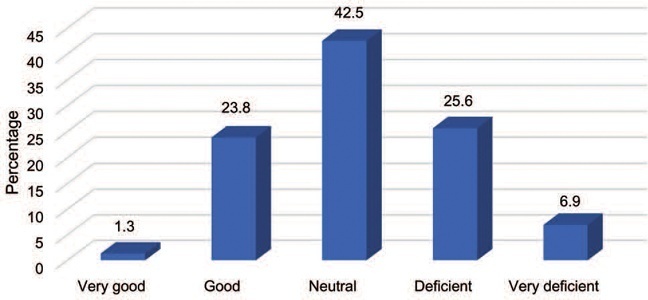
We collected survey results from 160 participants that met the inclusion criteria. Of those, 63.7% stated that the hospital where they work does not offer abortion training. Most of the participants consider that the position of the Peruvian government regarding therapeutic abortion is indifferent or deficient. The major limitations to provide therapeutic abortions included Peruvian law (53.8%), hospital policies (18.8%), and lack of experts (10.6%).
Most surveyed physicians supported therapeutic abortions and showed interest in improving their skills. However, not all hospitals offer training and education. The limited knowledge of the physicians regarding the law and institutional policies, as well as fear of ethical, legal, and religious repercussions, were the main barriers for providing abortions.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):586-592
To determine if there is a correlation between body mass index (BMI) and climacteric symptoms in postmenopausal women.
The study sample was composed of 109 postmenopausal women with a mean age of 57 ± 8 years, mean body mass index (BMI) of 30 ± 6 kg/m2, and 8 ± 8 years after menopause. For the assessment of the climacteric symptoms, the Blatt-Kupperman Index (BKI), the Menopause Rating Scale (MRS), and the Cervantes Scale (CS) were used. Data analysis was performed through the Chi-squared test, analysis of variance (ANOVA) with the Bonferroni post hoc test, and multiple linear regression. The level of significance adopted was of p < 0.05. The statistical analyses were performed using the Statistical Package for the Social Sciences (IBM SPSS Statistics for Windows, IBM Corp., Armonk, NY, United States) software, version 26.0.
The multiple linear regression showed a positive association (p<0.01) between BMI values and menopause symptoms when adjusted for age and time after menopause in the 3 questionnaires used (BKI: B = 0.432; CS: B = 304; and MRS: B = 302). Regarding symptom scores, the obese women had higher mean scores (p<0.05) when compared to eutrophic women (BKI = 28 ± 10 and 20 ± 10; and MRS = 20 ± 10 and 13±7, respectively). In the Chi-squared analysis, 28% of obese women had severe symptoms and 46% had moderate symptoms, while only 1% and 46% of eutrophic women had these same symptoms.
There is an association between BMI and climacteric symptoms, and overweight or obese women have more intense and moderate symptoms than eutrophic women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):845-853
To develop a protocol for hybrid low-risk prenatal care adapted to Brazilian guidelines, merging reduced face-to-face consultations and remote monitoring.
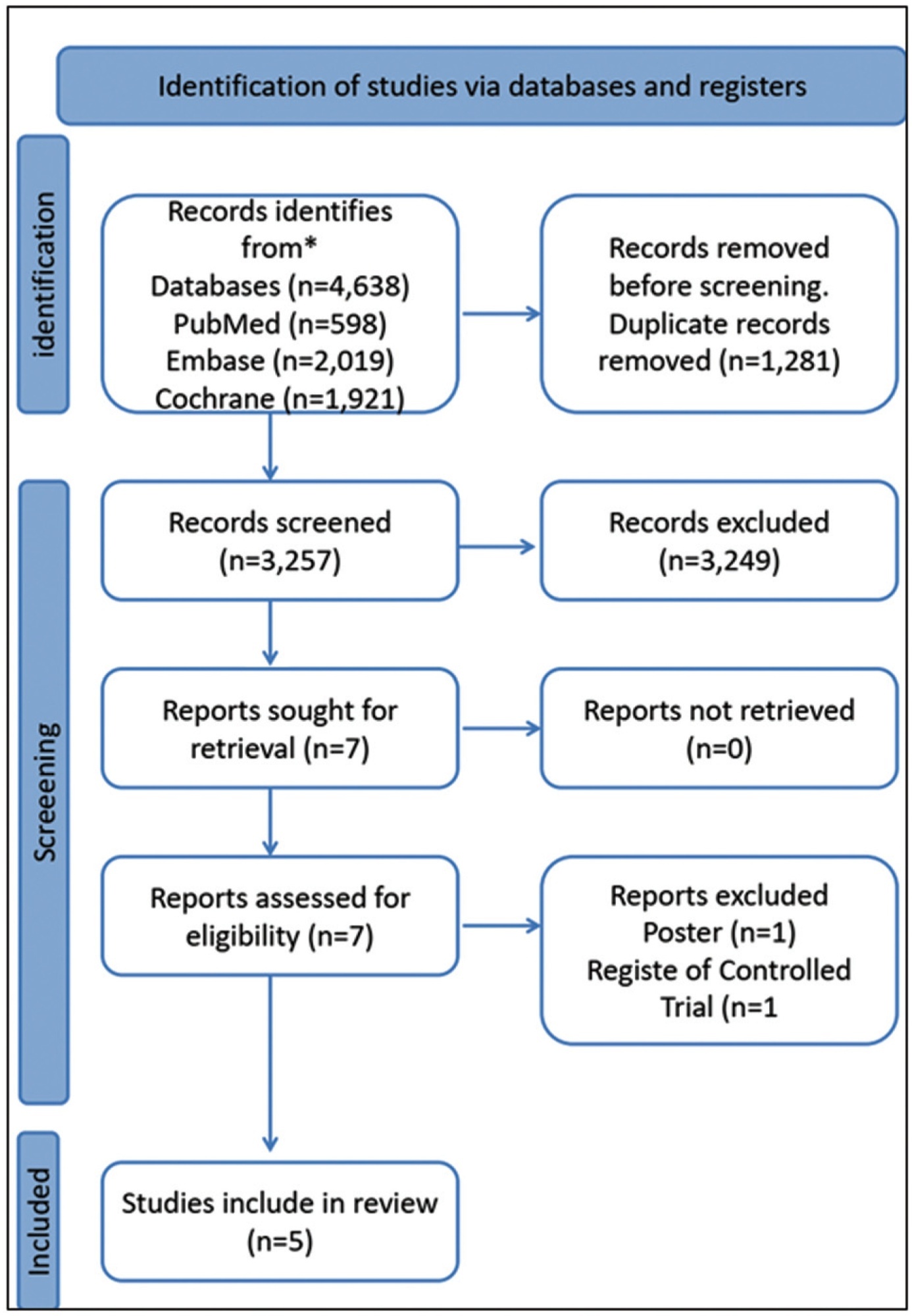
The PubMed, Embase, and Cochrane Library databases were systematically searched on telemedicine and antenatal care perspectives and adaptation of the low-risk prenatal care protocols recommended by the Ministry of Health and by the Brazilian Federation of Gynecology and Obstetrics Associations.
Five relevant articles and three manuals were included in the review, for presented criteria to develop this clinical guideline. We identified, in these studies, that the schedule of consultations is unevenly distributed among the gestational trimesters, and ranges from 7 to 14 appointments. In general, the authors propose one to two appointments in the first trimester, two to three appointments in the second trimester, and two to six appointments in the third trimester. Only three studies included puerperal evaluations. The routine exams recommended show minimal variations among authors. To date, there are no validated Brazilian protocols for prenatal care by telemedicine. The included studies showed that pregnant women were satisfied with this form of care, and the outcomes of interest, except for hypertensive diseases, were similar between the groups exposed to traditional and hybrid prenatal care.
The presented guideline comprises the Ministry of Health recommendations for low-risk prenatal care and reduces exposure to the hospital environment and care costs. A randomized clinical trial, to be developed by this group, will provide real-world data on safety, effectiveness, satisfaction, and costs.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(9):854-865
To comparatively evaluate the outcome of treatment with 150 versus 200 units (U) of botulinum toxin in achieving pain-free intercourse and relieving muscle contraction in order to allow gynecological examination.
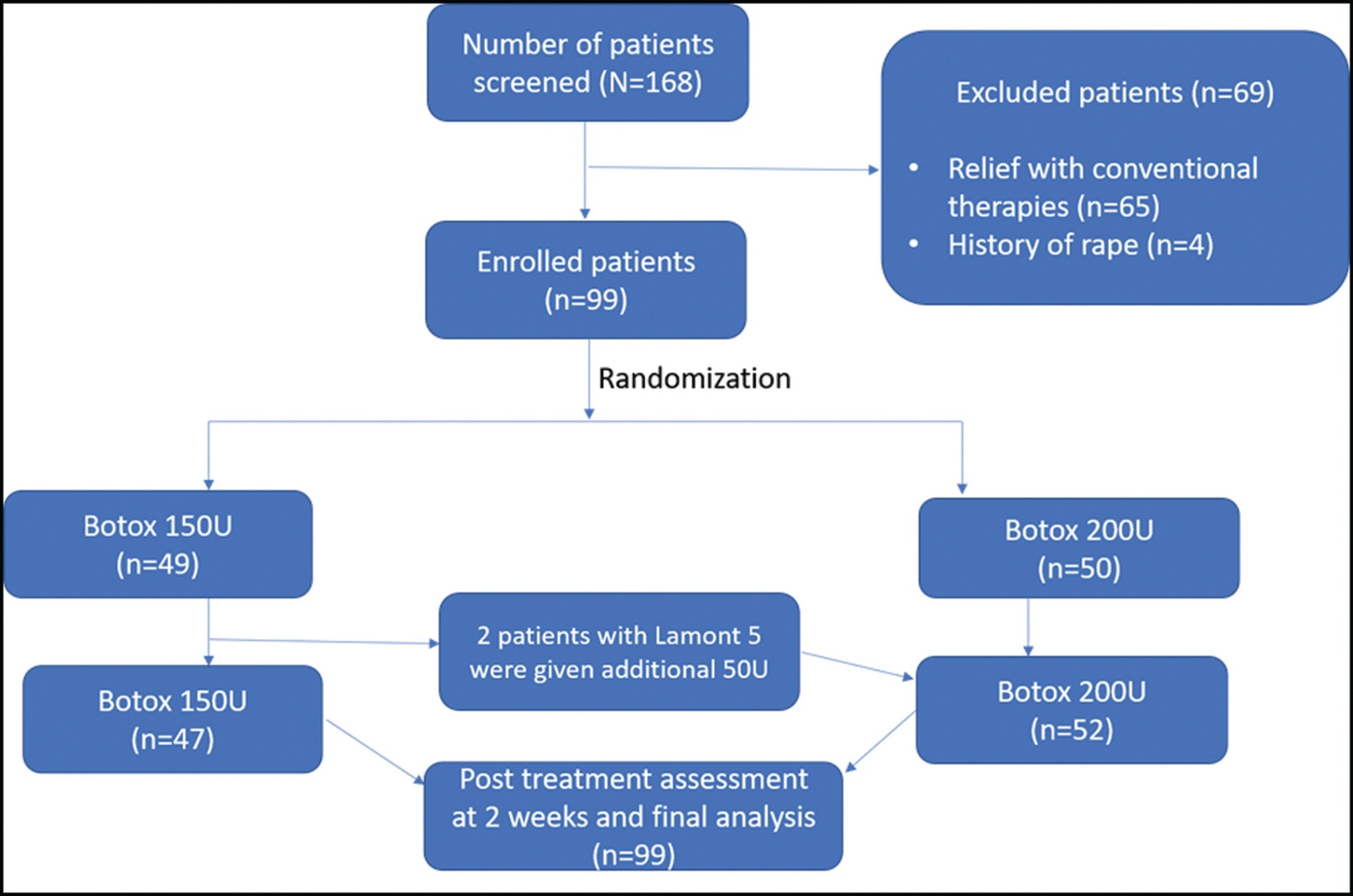
In this comparative prospective observational study, 99 patients with vaginismus were treated with botulinum toxin injections from September 2016 to August 2021. Diagnosis and grading of vaginismus severity were assessed using a Female Sexual Function Index (FSFI) questionnaire. Under local or general anesthesia, botulinum toxin diluted with preservative-free saline (150 U and 200 U) was injected into, above, and below the right and left bulbospongiosus muscle and the lateral submucosal areas of the introitus and perineal body using an insulin syringe. Patients were recalled after 2 weeks, and the postoperative outcome was recorded using a similar preoperative questionnaire.
Overall, the mean age of patients was 30.2 years. The baseline and clinical characteristics were comparable between the 2 groups (p > 0.05). Significant improvements were seen in the pain and anxiety scores of finger penetration, dilator use, intercourse, and cotton swab in individual groups. The intergroup comparisons between 150 U and 200 U of Botox were not statistically significant (p > 0.05).
Low-dose Botox (150 U) is equally effective as high dose Botox injections (200 U) in vaginismus patients. Therefore, Botox-150 U can be used to treat vaginismus as an alternative to high doses of the same substance.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(8):740-745
To assess the possible impact of the COVID-19 pandemic on maternal mortality among admissions for childbirth in 2020 in relation of the last 10 years.
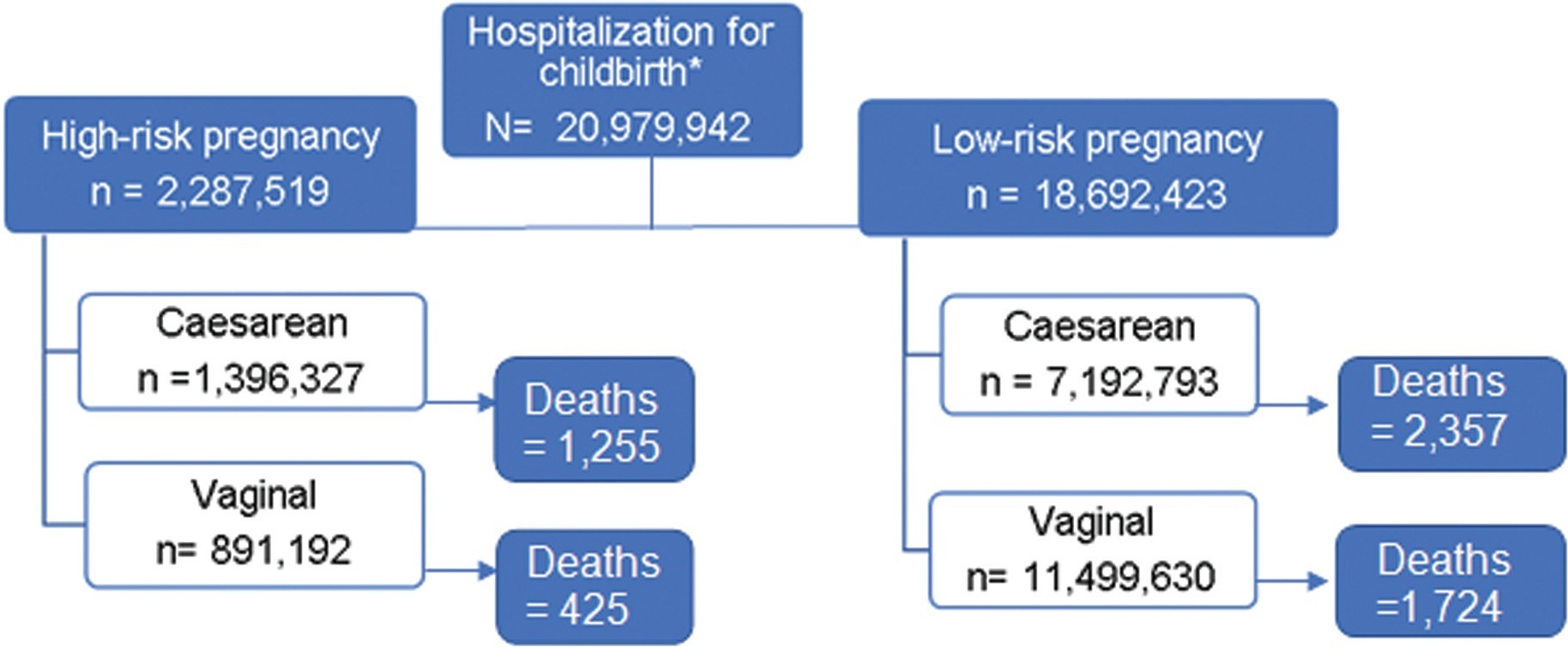
An ecological study with pregnant women who underwent hospital births at the Brazilian unified public health service (SUS, in the Portuguese acronym) in Brazil from 2010 to 2020. The mortality among admissions for childbirth was obtained based on the number of admissions for childbirth with reported death as outcome divided by the total number of admissions. The underlying gestational risk and route of delivery were considered based on the national surveillance system. The average mortality for the period between 2010 and 2019 (baseline) was compared with the rate of deaths in 2020 (1st pandemic year); the rate ratio was interpreted as the risk of death in 2020 in relation to the average of the previous period (RR), with 95% confidence intervals (CIs).
In 2020, the 1st year of the COVID-19 pandemic, 1,821,775 pregnant women were hospitalized for childbirth and 651 deaths were reported, which represents 8.7% of the total hospitalizations and 11.3% of maternal deaths between 2010 and 2020. There was an increase in maternal mortality after births in 2020 compared with the average for the period between 2010 and 2019, specially in low-risk pregnancies, both in vaginal (RR = 1.60; 95%CI:1.39–1.85) and cesarean births (RR = 1.18; 95%CI:1.04–1.34).
Maternal mortality among admissions for childbirth according to SUS data increased in 2020 compared with the average between 2010 and 2019, with an increment of 40% in low-risk pregnancies. The increase was of 18% after cesarean section and of 60% after vaginal delivery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):327-335
Determine the predictive criteria for success in inducing labor for live fetuses using misoprostol in pregnant women. Secondarily, the objective is to determine the rates of vaginal or cesarean delivery, duration of induction, interval of administration of misoprostol, the main causes of induction of labor and indication for operative delivery.
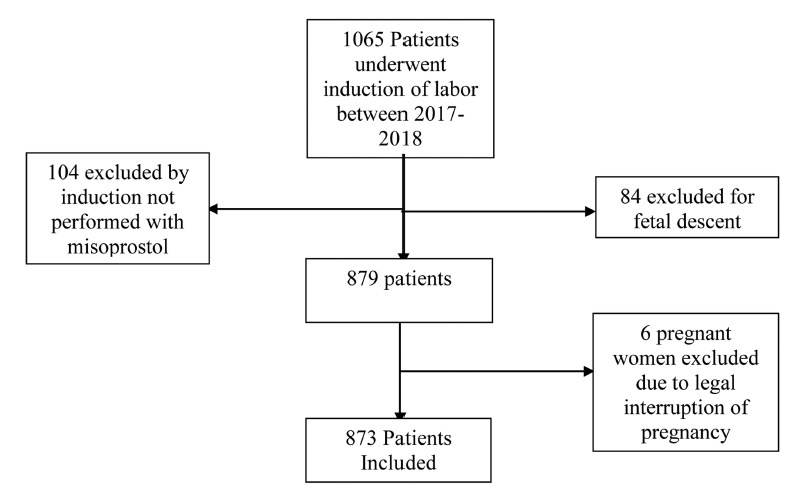
Medical records of 873 pregnant women admitted for cervical maturation from January 2017 to December 2018 were reviewed in a descriptive observational study of retrospective analysis, considering the following response variables: age, parity, Bishop Index, doses of misoprostol, labor induction time. Logistic regression models were used to predict success with misoprostol in non-operative deliveries.
Of the 873 patients evaluated, 72% evolved with vaginal delivery, 23% of the cases were cesarean, 5% forceps or vacuum-extractor. For non-operative delivery the predictive variables at admission were age, parity, gestational age and dilation. During hospitalization, fewer vaginal touches,amniotomy or amniorrhexis with clear fluid lead to a shorter induction time and a greater chance of non-operative delivery. False positives and false negatives of the model were always below 50% and correct answers above 65%.
At admission, age less than 24 years, previous normal births, lower the gestational age and greater the dilation, were predictive of greater probability of nonoperative delivery. During hospitalization, the less vaginal touches and occurrence of amniotomy/amniorrhexis with clear liquid indicate shorter induction time. Future studies with a prospective design and analysis of other factors are necessary to assess the replicability, generalization of these findings.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):369-375
To compare the oocyte maturation rate in the treatment of in vitro fertilization (IVF) in terms of the use of human chorionic gonadotropin (hCG), agonist gonadotropin-releasing hormone (GnRH) and dual trigger and to evaluate the associated risk factors for sub-optimal maturation rates.
A retrospective cohort study with 856 women who underwent IVF. They performed oocyte retrieval and were classified into 3 groups (1 - hCG, 2 - GnRHagonist, 3 - dual trigger). The primary outcome was maturation rate per trigger, and the secondary outcomes were the pregnancy rate per oocyte retrieval and the correlations between low maturation rate as well as the clinical and treatment characteristics of women.
The maturation rate was 77% in group 1; 76% in group 2, and 83% in group 3 (p=0.003). Group 2 showed women with better ovarian reserve, greater number of oocytes collected, and more mature oocytes and embryos compared with the other groups (p<0.001). The cumulative clinical pregnancy rate was no different between the groups (p=0.755). Low ovarian reserve and low doses of follicle-stimulating hormone (FSH) administered during the stimulus were associated with a higher chance of null maturation rate.
The oocyte maturation rates and IVF results were similar in all groups. Low ovarian reserve is associated with the worst treatment results.