Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo85
To evaluate the role of being human immunodeficiency virus (HIV) positive for predicting the risk of recurrence in women with a cervical high grade squamous intraepithelial lesion (HSIL) diagnosis.
Retrospective observational case-control study, comprising HIV positive (case) and HIV negative (control) women in a 1:4 ratio. Women assisted by the Erasto Gaertner Hospital, between 2009-2018, with cervical HSIL diagnosis, submitted to treatment by Loop electrosurgical excision procedure (LEEP), and with a minimum follow-up of 18 months, were included. The immunological status, number and time to recurrence were analyzed, with p<0.05 considered significant. In a second analysis, only patients with free margins were evaluated.
The sample consisted of 320 women (64 cases and 256 controls). Presence of HIV, CD4 levels <200 and detectable viral load (CV) were associated with high risk of recurrence, with odds ratio (OR) of 5.4 (p<0.001/95CI:2.8-10); 3.6 (p<0.001 /IC95:0.6-21.1) and 1.8 (p=0.039 /IC95:0.3-9.3), respectively. In the sample with free margins (n=271), this risk was also higher among seropositive patients, with OR 4.18 (p=0.001/95CI:1.8-9.2).
HIV is an independent risk factor for cervical HSIL recurrence and reduced disease-free survival time. Glandular involvement, compromised margins, undetectable CV and CD4<200 also increase the risk of relapse.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo44
To describe Top-hat results and their association with margin status and disease relapse in a referral facility in Brazil.
A retrospective study of 440 women submitted to LEEP to treat HSIL, in which 80 cases were complemented immediately by the top hat procedure (Top-hat Group - TH). TH Group was compared to women not submitted to Top-hat (NTH). The sample by convenience included all women that underwent LEEP from January 2017 to July 2020. The main outcome was the histological result. Other variables were margins, age, transformation zone (TZ), depth, and relapse. The analysis used the Chi-square test and logistic regression.
The TH Group was predominantly 40 and older (NTH 23.1% vs. TH 65.0%, p<0.001). No difference was found in having CIN2/CIN3 as the final diagnosis (NTH 17.0% vs. TH 21.3%, p=0.362), or in the prevalence of relapse (NTH 12.0% vs. TH 9.0%, p=0.482). Of the 80 patients submitted to top hat, the histological result was CIN2/CIN3 in eight. A negative top hat result was related to a negative endocervical margin of 83.3%. A CIN2/CIN3 Top-hat result was related to CIN2/CIN3 margin in 62.5% (p=0.009). The chance of obtaining a top hat negative result was 22.4 times higher (2.4-211.0) when the endocervical margin was negative and 14.5 times higher (1.5-140.7) when the ectocervical margin was negative.
The top hat procedure did not alter the final diagnosis of LEEP. No impact on relapse was observed. The procedure should be avoided in women of reproductive age.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):790-795
To compare cytological and histological results from women > 64 years old who followed the Brazilian national cervical cancer screening guidelines with those who did not.
The present observational retrospective study analyzed 207 abnormal cervical smear results from women > 64 years old in a mid-sized city in Brazil over 14 years. All results were reported according to the Bethesda System. The women were divided into those who followed the screening guidelines and those who did not.
Atypical squamous cells of undetermined significance and low-grade squamous intraepithelial lesion cytology results were found in 128 (62.2%) cases. Of these, 112 (87.5%) had repeated cytology with positive results. The other 79 (38.1%) with abnormal results should have been referred to colposcopy and biopsy. Out of 41 (51.9%) biopsied women, 23 (29.1%) had a confirmed diagnosis of neoplasia or precursor lesion. In contrast, among the 78 (37.7%) biopsied patients, 40 (51.3%) followed the guideline recommendations, with 9 (22.5%) positive biopsies. Of the 38 (48.7%) women who did not follow the guidelines, there were 24 (63.1%) positive results. Women who did not follow the guidelines demonstrated higher chances of cancer and precursor lesions (odds ratio [OR]: 5.904; 95% confidence interval [CI]: 2.188–15.932; p = 0.0002).
Women > 64 years old who did not follow the national screening protocol showed significant differences in the frequency of abnormal results and severity of diagnosis compared with those who followed the protocol.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(11):689-698
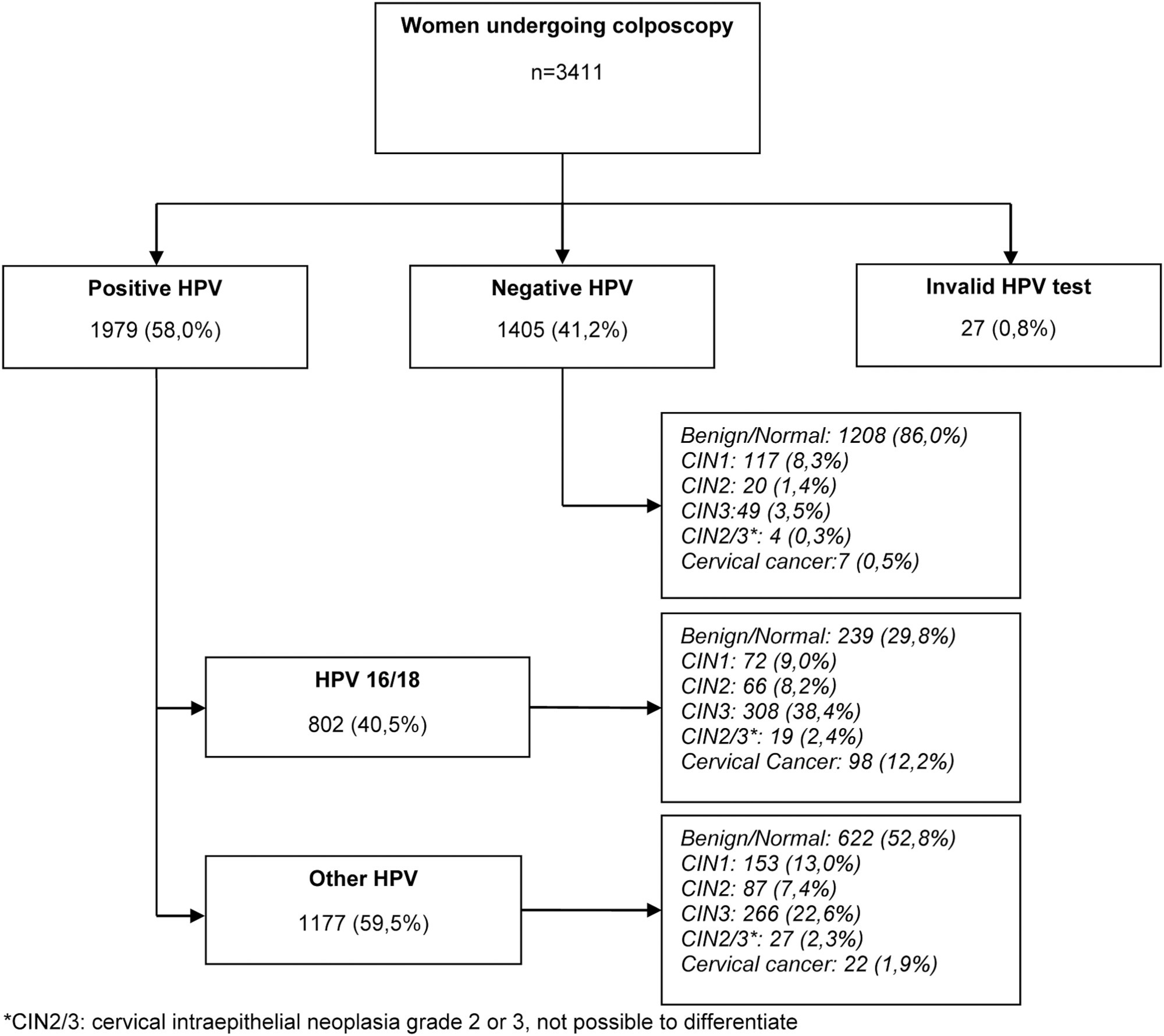
The present study aims to establish a risk profile for high-grade cervical lesions and cervical cancer (CIN2 + ) in women undergoing colposcopy at the Hospital do Câncer de Barretos, through the analysis of Human Papillomavirus (HPV) infection, cervical cytology, and patient's age.
Retrospective cross-sectional study based on a computerized database of women aged ≥ 18 years old who underwent colposcopy at the Prevention Department of the Hospital do Câncer de Barretos from 2017 to 2019.
A total of 3,411 women were included, 58.0% were positive for high-risk-HPV test, with a higher prevalence of CIN2+ for HPV16 (30.3%) and other HPV (45.0%). Cytological findings that suggest invasive cervical cancer (squamous cells or adenocarcinoma), regardless of the status of HPV test, showed 100% diagnosis of CIN2 + , while atypias that suggest high-grade lesions, HSIL and ASC-H, positive for HPV test, showed in 86 and 55.2%, respectively, diagnosis of CIN2 + . ASC-H cytological results among women aged > 40 years old and negative HPV were mainly associated with benign findings. We observed that ≤ CIN1 has a higher prevalence among older women with negative HPV, while for high-grade lesions there is an increase among young women HPV16- and/or 18-positive. In cancer diagnosis, we observed a predominance of HPV 16/18 regardless of the age group.
The highest risks of precursor lesions and cervical cancer were found among women with positive HPV 16/18 tests and severe cytological atypia in population screening tests. In addition, cytological findings of ASC-H HPV negative in women > 40 years old usually represent benign findings in histological investigation.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(5):235-241
To evaluate the accuracy and patient acceptability toward self-sampling using a new device - SelfCervix® - for detecting HPV-DNA.
A total of 73 women aged 25–65 who underwent regular cervical cancer screening from March to October 2016 were included. Women performed self-sampling followed by a physician-sampling, and the samples were analyzed for HPV-DNA. After that, patients were surveyed about their acceptability of self-sampling.
HPV-DNA detection rate of self-sampling presented high accuracy and was similar to physician-collection. Sixty-four (87.7%) patients answered the acceptability survey. Most patients (89%) considered the self-sampling comfortable, and 82.5% preferred self-sampling to physician-sampling. The reasons cited were time-saving and convenience. Fifty-one (79.7%) reported that they would recommend self-sampling.
Self-sampling using the new Brazilian device SelfCervix® is not inferior in HPV-DNA detection rate compared with physician-collection, and patients are supportive of the method. Therefore, it might be an option to reach under-screened populations in Brazil.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(4):201-206
To evaluate recurrence rates and risk factors among women with stage IA1 cervical cancer without lymph vascular space invasion managed conservatively.
retrospective review of women with stage IA1 squamous cervical cancer who underwent cold knife cone or loop electrosurgical excision procedure, between 1994 and 2015, at a gynecologic oncology center in Southern Brazil. Age at diagnosis, pre-conization findings, conization method, margin status, residual disease, recurrence and survival rates were collected and analyzed.
26 women diagnosed with stage IA1 squamous cervical cancer without lymphovascular space invasion underwent conservative management and had at least 12 months follow-up. The mean follow-up was 44.6 months. The mean age at diagnosis was 40.9 years. Median first intercourse occurred at age 16 years, 11.5% were nulliparous and 30.8% were current or past tobacco smokers. There was one Human immunodeficiency virus positive patient diagnosed with cervical intraepithelial neoplasia grade 2 at 30 months after surgery. However, there were no patients diagnosed with recurrent invasive cervical cancer and there were no deaths due to cervical cancer or other causes in the cohort.
Excellent outcomes were noted in women with stage IA1 cervical cancer without lymphovascular space invasion and with negative margins who were managed conservatively, even in a developing country.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(8):790-796
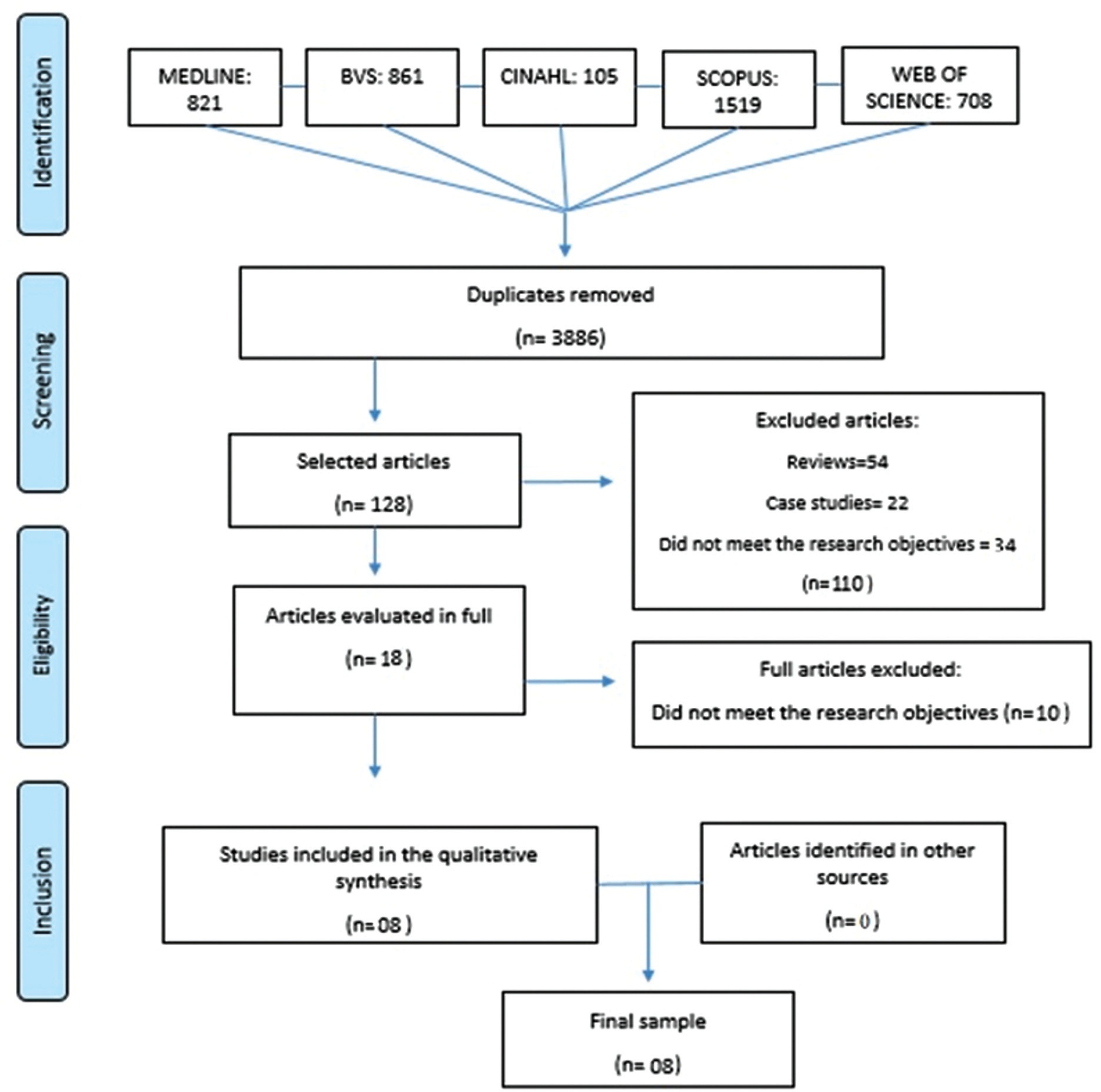
This systematic review aims at describing the prevalence of urinary and sexual symptoms among women who underwent a hysterectomy for cervical cancer.
A systematic search in six electronic databases was performed, in September 2019, by two researchers. The text search was limited to the investigation of prevalence or occurrence of lower urinary tract symptoms (LUTS) and sexual dysfunctions in women who underwent a hysterectomy for cervical cancer. For search strategies, specific combinations of terms were used.
A total of 8 studies, published between 2010 and 2018, were included in the sample. The average age of the participants ranged from 40 to 56 years, and the dysfunctions predominantly investigated in the articles were urinary symptoms (n= 8). The rates of urinary incontinence due to radical abdominal hysterectomy ranged from 7 to 31%. The same dysfunction related to laparoscopic radical hysterectomy varied from 25 to 35% and to laparoscopic nerve sparing radical hysterectomy varied from 25 to 47%. Nocturia ranged from 13%, before treatment, to 30%, after radical hysterectomy. The prevalence rates of dyspareunia related to laparoscopic radical hysterectomy and laparoscopic nerve sparing radical hysterectomy ranged from 5 to 16% and 7 to 19% respectively. The difficulty in having orgasm was related to laparoscopic radical hysterectomy (10 to 14%) and laparoscopic nerve sparing radical hysterectomy (9 to 19%).
Urinary and sexual dysfunctions after radical hysterectomy to treat cervical cancer are frequent events. The main reported disorders were urinary incontinence and dyspareunia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):264-271
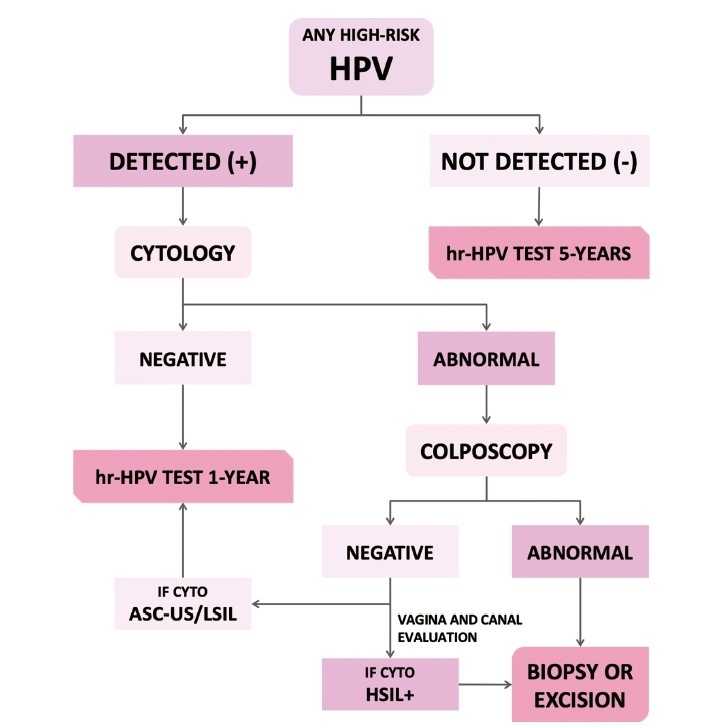
The present update is a reassessment of the 2018 ‘Guidelines for HPV-DNA Testing for Cervical Cancer Screening in Brazil’ (Zeferino et al.)9, according to the changes observed in new international guidelines and knowledge updates. The most relevant and recent guidelines were assessed. Questions regarding the clinical practice were formulated, and the answers considered the perspective of the public and private sectors of the Brazilian health system. The review addressed risk-based strategies regarding age to start and stop screening, the use of cytology and colposcopy to support management decisions, treatment, follow-up strategies, and screening in specific groups, including vaccinated women. The update aims to improve the prevention of cervical cancer and to reduce overtreatment and the misuse of HPV testing.