Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(10):749-751
DOI 10.1590/S0100-72032003001000009
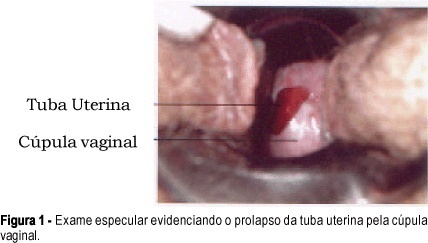
Fallopian tube prolapse is a rare complication after hysterectomy, with approximately 80 cases described in the literature. The symptoms are nonspecific including vaginal bleeding, dyspareunia and chronic pelvic pain. The differential diagnosis must be done with granulation tissue of the vaginal cuff and vaginal carcinoma. The treatment should be individualized, and is possible to be done by vaginal, abdominal or laparoscopic approach. We report a case of a 47-year-old woman with myoma who was submitted to a vaginal hysterectomy and evolved with fallopian tube prolapse 11 months after surgery. Specular examination showed a fungating, friable and bleeding lesion at the vaginal cuff. The clinical findings suggested the diagnosis of fallopian tube prolapse. The patient was submitted to a new surgical intervention with resection of the left fallopian tube. The histologic examination confirmed the diagnosis and the patient evolved with complete remission of the symptoms.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(7):443-448
DOI 10.1590/S0100-72032000000700007
Purpose: to determine the main factors associated with the occurrence of surgical site infection in patients submitted to total abdominal hysterectomy at the Instituto Materno ¾ Infantil de Pernambuco (iMIP). Methods: a cross-sectional study was conducted, enrolling patients submitted to total abdominal hysterectomy at IMIP who returned to postsurgical consultation for infection control, between January, 1995 and December, 1998 (n = 414). The frequency of surgical site infection (defined according to the CDC criteria, 1998) was 10% (42 cases). Prevalence risk (PR) of infection (dependent variable) and its 95% confidence interval (CI) were calculated for independent variables: age, obesity, hypertension, diabetes, malignant pathology, type of incision, duration of surgery and antibiotic prophylaxis. Multiple logistic regression analysis was used to determine adjusted risk of infection. Results: a significantly increased risk of infection was found for the following variables: age >60 years (PR = 2.39, 95% CI = 1.15-4.94), obesity (PR = 3.2, 95% CI = 1.83-5.59), duration of surgery >2 hours (PR = 2.35, 95% CI = 1.32-4.21) and diabetes (PR = 6.0, 95% CI = 3.41-10.57). On the other hand, risk of infection was significantly reduced when antibiotic prophylaxis was administered (PR = 0.38, 95% CI = 0.21-0.68). Type of incision, malignant disease and hypertension were not associated with infection. Conclusions: the factors associated with increased risk of surgical site infection after total abdominal hysterectomy at IMIP were: age >60 years, obesity, diabetes and surgical duration >2 hours. Antibiotic prophylaxis showed a protective effect with reduction of risk of infection.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(3):169-176
DOI 10.1590/S0100-72032003000300005
PURPOSE: to compare intra- and postoperative results of vaginal hysterectomy with those of abdominal hysterectomy in women without genital prolapse or adnexal pathology. METHODS: a randomized, open clinical trial was conducted, involving 35 patients without genital prolapse scheduled for total hysterectomy due to benign disease, at IMIP, Recife, Brazil. These patients were randomly assigned to vaginal hysterectomy (19 patients) or abdominal hysterectomy (16 patients). Main outcome measures included estimated blood loss, rate of blood transfusion, duration of surgery, postoperative pain (intensity and analgesic requirement), time in hospital, postoperative complications, recovery time and patient satisfaction. Statistical analysis was performed using chi2, exact Fisher and Mann-Whitney tests at a 5% level of significance. RESULTS: estimated blood losses were significantly lower in vaginal hysterectomy (median of 520 mL) than in abdominal hysterectomy (median 902 mL). There was no blood transfusion among patients of the vaginal hysterectomy group, in contrast to 19% of the abdominal hysterectomy group. Duration of surgery was similar (median of 120 min in both groups). Postoperative pain, as measured by visual analog scale and analgesic requirement, was lower for vaginal hysterectomy than for abdominal hysterectomy. There was no statistically significant difference regarding frequency of postoperative complications. There was one case of infection in each group and one case of thrombosis in the vaginal hysterectomy group. Postoperative hospital stay was shorter in the vaginal group. Recovery time was significantly shorter in the vaginal group (median of 35 days) versus the abdominal group (median 40 days). Overall patient satisfaction with the operation was similar in the two groups. CONCLUSIONS: patients without genital prolapse submitted to vaginal hysterectomy for treatment of benign diseases had some advantages in relation to those submitted to abdominal hysterectomy: lower intraoperative blood loss, lower postoperative pain and faster recovery time. Vaginal hysterectomy may replace abdominal hysterectomy in most patients who require hysterectomy.